Volume 12, Issue 1 (6-2026)
J Sport Biomech 2026, 12(1): 136-153 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mansoori M, Ilbeigi S, Fatahi A. Effects of Vestibular Disturbances on Lower-Limb Muscle Activation in Active Children During the Stance Phase of Gait. J Sport Biomech 2026; 12 (1) :136-153
URL: http://biomechanics.iauh.ac.ir/article-1-435-en.html
URL: http://biomechanics.iauh.ac.ir/article-1-435-en.html
1- Department of Physical Education and Sport Sciences, Central Tehran Branch, Islamic Azad University, Tehran, Iran.
2- Department of Sports Sciences, University of Birjand, Birjand, Iran.
2- Department of Sports Sciences, University of Birjand, Birjand, Iran.
Full-Text [PDF 2007 kb]
(9 Downloads)
| Abstract (HTML) (16 Views)
Full-Text: (4 Views)
Extended Abstract
1. Introduction
Gait is a complex human movement that relies on the coordinated activation of multiple muscle groups across the ankle, knee, and hip joints (1). Beyond examining gait in healthy individuals, researchers also analyze gait under various neural conditions and external stimulations (3). Once initiated, gait emerges as a repetitive pattern of lower-limb movements that transitions naturally from standing to stepping with minimal attentional demand (3). Several factors, including gender, physical fitness, and age, can influence the execution and quality of these movement patterns (2). Balance control is a fundamental component of motor function and plays a crucial role in nearly all daily activities (4). Disruptions in balance can impair other motor abilities, such as sensory integration and neuromuscular coordination (5). The vestibular system—comprising structures of the inner ear and associated neural pathways—contributes significantly to postural control, eye–head coordination, and spatial orientation, thereby helping maintain overall body stability (6). Understanding factors that affect balance is critical for reducing fall risk across the lifespan. Muscle weakness, particularly with aging, can compromise mechanical muscle function and elevate the likelihood of falls. Key lower-limb muscles such as the quadriceps, hamstrings, and gastrocnemius contribute to knee-joint stability, and alterations in their activation patterns can modify joint loading and movement efficiency (11, 12, 13). Electromyographic (EMG) analysis is widely employed in gait research as it provides valuable insights into neuromuscular contributions to biomechanical events. Given the central role of the vestibular system in maintaining postural stability, the present study aims to examine the effects of vestibular stimulation on the electrical activity of selected lower-limb muscles in active children during the stance phase of gait.
2. Methods
This study included 30 active children aged 7–11 years from Tehran who participated in sports at least three times per week. The sample size was determined using G*Power with a statistical power of 0.80, an alpha level of 0.05, and an effect size of 0.50. Participants were screened to ensure the absence of underlying medical conditions, postural abnormalities, or lower-limb injuries (26). All ethical requirements were fulfilled, and written informed consent was obtained from both the children and their parents or guardians (IR.SSRC.REC.1403.005). An 8-channel surface electromyography system (MEGADOWIN 6000ME, Finland) with a 1000 Hz sampling frequency was used to record muscle activity. Disposable electrodes were placed over the biceps femoris, rectus femoris, gastrocnemius, soleus, tibialis anterior, and peroneus longus muscles according to the SENIAM guidelines, with a 2-cm inter-electrode distance following standard skin preparation (17). The protocol began with a pre-test session during which participants performed three maximal voluntary isometric contractions for each muscle. They then walked along a designated pathway six times (three trials with eyes open and three with eyes closed). A post-test session was conducted one day later. In this session, participants again walked the same pathway six times (three with eyes open and three with eyes closed), but only after receiving vestibular perturbation induced by controlled rotation on a turntable (five clockwise rotations and five counterclockwise rotations) (18). EMG signals were processed using a 10–500 Hz band-pass filter and a 50 Hz notch filter. The data were smoothed and normalized using the root mean square (RMS) method. Statistical analyses included descriptive statistics, the Kolmogorov–Smirnov test, repeated-measures ANOVA, and MANOVA, performed in SPSS version 22. The significance level was set at p < 0.05.
1. Introduction
Gait is a complex human movement that relies on the coordinated activation of multiple muscle groups across the ankle, knee, and hip joints (1). Beyond examining gait in healthy individuals, researchers also analyze gait under various neural conditions and external stimulations (3). Once initiated, gait emerges as a repetitive pattern of lower-limb movements that transitions naturally from standing to stepping with minimal attentional demand (3). Several factors, including gender, physical fitness, and age, can influence the execution and quality of these movement patterns (2). Balance control is a fundamental component of motor function and plays a crucial role in nearly all daily activities (4). Disruptions in balance can impair other motor abilities, such as sensory integration and neuromuscular coordination (5). The vestibular system—comprising structures of the inner ear and associated neural pathways—contributes significantly to postural control, eye–head coordination, and spatial orientation, thereby helping maintain overall body stability (6). Understanding factors that affect balance is critical for reducing fall risk across the lifespan. Muscle weakness, particularly with aging, can compromise mechanical muscle function and elevate the likelihood of falls. Key lower-limb muscles such as the quadriceps, hamstrings, and gastrocnemius contribute to knee-joint stability, and alterations in their activation patterns can modify joint loading and movement efficiency (11, 12, 13). Electromyographic (EMG) analysis is widely employed in gait research as it provides valuable insights into neuromuscular contributions to biomechanical events. Given the central role of the vestibular system in maintaining postural stability, the present study aims to examine the effects of vestibular stimulation on the electrical activity of selected lower-limb muscles in active children during the stance phase of gait.
2. Methods
This study included 30 active children aged 7–11 years from Tehran who participated in sports at least three times per week. The sample size was determined using G*Power with a statistical power of 0.80, an alpha level of 0.05, and an effect size of 0.50. Participants were screened to ensure the absence of underlying medical conditions, postural abnormalities, or lower-limb injuries (26). All ethical requirements were fulfilled, and written informed consent was obtained from both the children and their parents or guardians (IR.SSRC.REC.1403.005). An 8-channel surface electromyography system (MEGADOWIN 6000ME, Finland) with a 1000 Hz sampling frequency was used to record muscle activity. Disposable electrodes were placed over the biceps femoris, rectus femoris, gastrocnemius, soleus, tibialis anterior, and peroneus longus muscles according to the SENIAM guidelines, with a 2-cm inter-electrode distance following standard skin preparation (17). The protocol began with a pre-test session during which participants performed three maximal voluntary isometric contractions for each muscle. They then walked along a designated pathway six times (three trials with eyes open and three with eyes closed). A post-test session was conducted one day later. In this session, participants again walked the same pathway six times (three with eyes open and three with eyes closed), but only after receiving vestibular perturbation induced by controlled rotation on a turntable (five clockwise rotations and five counterclockwise rotations) (18). EMG signals were processed using a 10–500 Hz band-pass filter and a 50 Hz notch filter. The data were smoothed and normalized using the root mean square (RMS) method. Statistical analyses included descriptive statistics, the Kolmogorov–Smirnov test, repeated-measures ANOVA, and MANOVA, performed in SPSS version 22. The significance level was set at p < 0.05.
3. Results
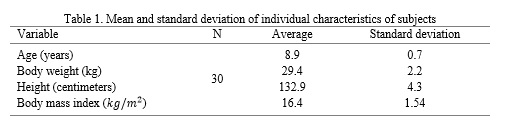
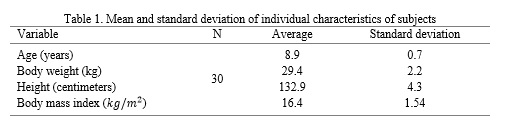
The demographic characteristics of the children participating in this study are summarized in Table 1. The mean age of the participants was 8.9 ± 0.7 years, with an average body mass of 29.4 ± 2.2 kg and a mean height of 132.9 ± 4.3 cm. The mean BMI was 16.4 ± 1.54 kg/m², indicating that the children fell within a healthy range for their age group. This homogeneity in anthropometric characteristics ensured that differences in muscle activity were primarily attributable to sensory conditions rather than physical disparities among subjects.
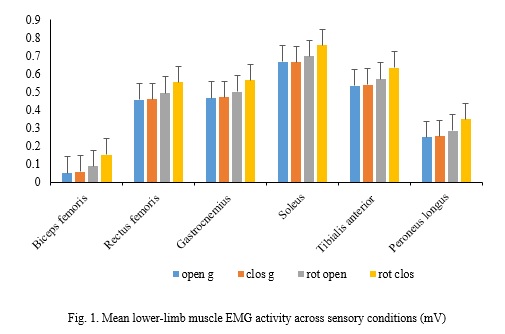
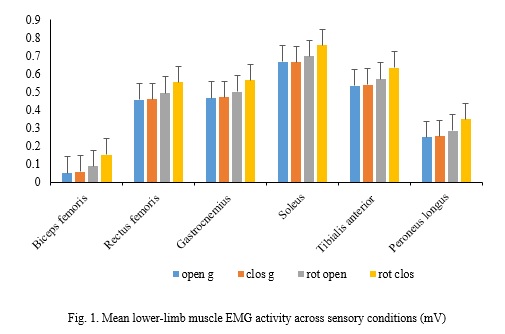
Patterns of muscle activation across the four sensory conditions are illustrated in Fig. 1. Vestibular perturbation clearly influenced the electrical activity of lower-limb muscles during the stance phase of gait. Among the four conditions examined, the eyes-closed with vestibular perturbation condition elicited the highest neuromuscular demand. This was reflected in substantial increases in muscle activation, particularly in muscles responsible for postural stabilization and maintenance of mediolateral balance. As shown in Fig. 1, the soleus muscle demonstrated the greatest response to vestibular challenges, reaching a mean activation of 0.7572 mV/s. This elevated activity suggests that children relied heavily on the ankle plantarflexors to compensate for the reduced reliability of vestibular and visual input. Increased activation was also observed in the biceps femoris and peroneus longus, indicating enhanced recruitment of both posterior-chain and lateral stabilizing muscles when balance became more challenging. Statistical analyses confirmed that the differences in muscle activity across the sensory conditions were significant at p < 0.01. This finding indicates that vestibular disturbances produced measurable and meaningful alterations in neuromuscular control during the stance phase of walking. The consistent rise in muscle activation under perturbed conditions—particularly in the absence of vision—reflects the increased postural difficulty imposed by reduced vestibular function. Overall, the findings depicted in Fig. 1 demonstrate that vestibular perturbation disrupts normal gait regulation, prompting children to increase activation in specific lower-limb muscles involved in stability, joint protection, and control of sway. These results highlight the essential contribution of vestibular input to maintaining coordinated muscle function during gait and underscore the susceptibility of children’s neuromuscular systems to balance-related challenges.
4. Discussion
This study investigated the influence of vestibular perturbations on lower-limb muscle activity in children during gait. The findings demonstrated significant increases in the activation of the biceps femoris, soleus, and peroneus longus muscles, indicating that the vestibular system plays a central role in dynamic balance regulation. When vestibular input becomes unreliable, the body activates compensatory neuromuscular mechanisms to maintain postural stability, leading to heightened muscle activity—an observation consistent with previous research (28).
Earlier studies have shown that targeted vestibular stimulation can enhance balance performance in children with vestibular dysfunction (28), and that visual input serves as a critical source of sensory information for postural control (29). As balance ability improves progressively between the ages of 3 and 19 years (30), the developmental stage of the children in this study may explain their pronounced reliance on multisensory integration during gait. Evidence also suggests that short-term vestibular-based interventions enhance motor performance in children with neurological conditions, such as cerebral palsy (31), while external noisy stimulation can modify muscle activation patterns (32). Such findings collectively emphasize the importance of accurate vestibular signaling for both cognitive and motor development (33). Interventions combining vestibular and neuromuscular training have been shown to benefit children with Down syndrome (34), and structured programs such as FIFA 11+ effectively improve balance and reduce musculoskeletal injuries (35). However, some studies have reported conflicting results, often due to differences in participant characteristics, methodological approaches, or the type and intensity of sensory challenges used (36, 37). In the present study, removing visual input alone produced minimal effects on muscle activity, whereas the combination of visual deprivation and vestibular disturbance led to substantial increases. This demonstrates the cumulative effect of multi-sensory disruption on neuromuscular responses. These results highlight the importance of strengthening sensory systems during childhood to support lifelong motor health and reduce the risk of functional decline later in life. Prior work suggests that vestibular inputs contribute not only to balance but also to spatial perception and cortical processing (38). Additionally, targeted vestibular exercises have been shown to improve balance and coordination in children with attention-deficit/hyperactivity disorder (39). Biomechanical research also indicates that disruptions in sensory feedback can alter muscle efficiency and movement patterns, influencing joint loading and gait stability (40–42). Given that balance is governed by the interaction of vestibular, visual, and proprioceptive inputs (43, 44), assessing vestibular function in children may reveal underlying motor control vulnerabilities and support early rehabilitation planning (45–48). Overall, the present findings demonstrate that vestibular perturbations significantly reshape muscle activation strategies during gait, reflecting the body’s adaptive attempts to preserve stability when sensory reliability is compromised.
Ethical Considerations
Compliance with ethical guidelines
This study was conducted in accordance with established ethical standards for research involving human participants. The study protocol was reviewed and approved by the Research Ethics Committee of the Sports Science Research Institute (IR.SSRC.REC.1403.005). In line with these guidelines, written informed consent was obtained from all participating children and their parents or legal guardians.
Funding
This research did not receive any grants from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception, design, data collection, analysis, and preparation of the manuscript.
Conflicts of interest
The authors declare that they have no conflicts of interest related to this study.
The demographic characteristics of the children participating in this study are summarized in Table 1. The mean age of the participants was 8.9 ± 0.7 years, with an average body mass of 29.4 ± 2.2 kg and a mean height of 132.9 ± 4.3 cm. The mean BMI was 16.4 ± 1.54 kg/m², indicating that the children fell within a healthy range for their age group. This homogeneity in anthropometric characteristics ensured that differences in muscle activity were primarily attributable to sensory conditions rather than physical disparities among subjects.
Patterns of muscle activation across the four sensory conditions are illustrated in Fig. 1. Vestibular perturbation clearly influenced the electrical activity of lower-limb muscles during the stance phase of gait. Among the four conditions examined, the eyes-closed with vestibular perturbation condition elicited the highest neuromuscular demand. This was reflected in substantial increases in muscle activation, particularly in muscles responsible for postural stabilization and maintenance of mediolateral balance. As shown in Fig. 1, the soleus muscle demonstrated the greatest response to vestibular challenges, reaching a mean activation of 0.7572 mV/s. This elevated activity suggests that children relied heavily on the ankle plantarflexors to compensate for the reduced reliability of vestibular and visual input. Increased activation was also observed in the biceps femoris and peroneus longus, indicating enhanced recruitment of both posterior-chain and lateral stabilizing muscles when balance became more challenging. Statistical analyses confirmed that the differences in muscle activity across the sensory conditions were significant at p < 0.01. This finding indicates that vestibular disturbances produced measurable and meaningful alterations in neuromuscular control during the stance phase of walking. The consistent rise in muscle activation under perturbed conditions—particularly in the absence of vision—reflects the increased postural difficulty imposed by reduced vestibular function. Overall, the findings depicted in Fig. 1 demonstrate that vestibular perturbation disrupts normal gait regulation, prompting children to increase activation in specific lower-limb muscles involved in stability, joint protection, and control of sway. These results highlight the essential contribution of vestibular input to maintaining coordinated muscle function during gait and underscore the susceptibility of children’s neuromuscular systems to balance-related challenges.
4. Discussion
This study investigated the influence of vestibular perturbations on lower-limb muscle activity in children during gait. The findings demonstrated significant increases in the activation of the biceps femoris, soleus, and peroneus longus muscles, indicating that the vestibular system plays a central role in dynamic balance regulation. When vestibular input becomes unreliable, the body activates compensatory neuromuscular mechanisms to maintain postural stability, leading to heightened muscle activity—an observation consistent with previous research (28).
Earlier studies have shown that targeted vestibular stimulation can enhance balance performance in children with vestibular dysfunction (28), and that visual input serves as a critical source of sensory information for postural control (29). As balance ability improves progressively between the ages of 3 and 19 years (30), the developmental stage of the children in this study may explain their pronounced reliance on multisensory integration during gait. Evidence also suggests that short-term vestibular-based interventions enhance motor performance in children with neurological conditions, such as cerebral palsy (31), while external noisy stimulation can modify muscle activation patterns (32). Such findings collectively emphasize the importance of accurate vestibular signaling for both cognitive and motor development (33). Interventions combining vestibular and neuromuscular training have been shown to benefit children with Down syndrome (34), and structured programs such as FIFA 11+ effectively improve balance and reduce musculoskeletal injuries (35). However, some studies have reported conflicting results, often due to differences in participant characteristics, methodological approaches, or the type and intensity of sensory challenges used (36, 37). In the present study, removing visual input alone produced minimal effects on muscle activity, whereas the combination of visual deprivation and vestibular disturbance led to substantial increases. This demonstrates the cumulative effect of multi-sensory disruption on neuromuscular responses. These results highlight the importance of strengthening sensory systems during childhood to support lifelong motor health and reduce the risk of functional decline later in life. Prior work suggests that vestibular inputs contribute not only to balance but also to spatial perception and cortical processing (38). Additionally, targeted vestibular exercises have been shown to improve balance and coordination in children with attention-deficit/hyperactivity disorder (39). Biomechanical research also indicates that disruptions in sensory feedback can alter muscle efficiency and movement patterns, influencing joint loading and gait stability (40–42). Given that balance is governed by the interaction of vestibular, visual, and proprioceptive inputs (43, 44), assessing vestibular function in children may reveal underlying motor control vulnerabilities and support early rehabilitation planning (45–48). Overall, the present findings demonstrate that vestibular perturbations significantly reshape muscle activation strategies during gait, reflecting the body’s adaptive attempts to preserve stability when sensory reliability is compromised.
Ethical Considerations
Compliance with ethical guidelines
This study was conducted in accordance with established ethical standards for research involving human participants. The study protocol was reviewed and approved by the Research Ethics Committee of the Sports Science Research Institute (IR.SSRC.REC.1403.005). In line with these guidelines, written informed consent was obtained from all participating children and their parents or legal guardians.
Funding
This research did not receive any grants from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception, design, data collection, analysis, and preparation of the manuscript.
Conflicts of interest
The authors declare that they have no conflicts of interest related to this study.
Type of Study: Research |
Subject:
Special
Received: 2025/09/4 | Accepted: 2025/11/16 | Published: 2025/11/17
Received: 2025/09/4 | Accepted: 2025/11/16 | Published: 2025/11/17
References
1. Zajac FE, Neptune RR, Kautz SA. Biomechanics and muscle coordination of human walking: Lessons from dynamical simulations and clinical implications. Gait and Posture. 2003;17(1):1-17. [DOI:10.1016/S0966-6362(02)00069-3] [PMID]
2. Kerkman JN, Bekius A, Boonstra TW, Daffertshofer A, Dominici N. Muscle synergies and coherence networks reflect different modes of coordination during walking. Frontiers in Physiology. 2020;11:751. [DOI:10.3389/fphys.2020.00751] [PMID]
3. Mickelborough J, van der Linden ML, Tallis RC, Ennos AR. Muscle activity during gait initiation in normal elderly people. Gait and Posture. 2004;19(1):50-57. [DOI:10.1016/S0966-6362(03)00016-X] [PMID]
4. Rajabi S, Goodarzi B, Mazidi M. The comparison effects of eight weeks spark and Frenkel exercises on static and dynamic balance in the blinds. Hormozgan Medical Journal. 2017;20(6):373-380. [DOI:10.18869/acadpub.hmj.20.6.401]
5. Božanić Urbančič N, Battelino S, Vozel D. Appropriate vestibular stimulation in children and adolescents-A prerequisite for normal cognitive, motor development and bodily homeostasis: A review. Children. 2023;11(1):2. [DOI:10.3390/children11010002] [PMID]
6. Porto JM, Cangussu-Oliveira LM, Freire Júnior RC, Vieira FT, Capato LL, et al. Relationship between lower limb muscle strength and future falls among community-dwelling older adults with no history of falls: A prospective 1-year study. Journal of Applied Gerontology. 2021;40(3):339-346. [DOI:10.1177/0733464820932778] [PMID]
7. Goldberg JM. Vestibular inputs: The vestibular system. In: Pfaff DW, editor. Neuroscience in the 21st Century: From Basic to Clinical. Cham: Springer International Publishing; 2022;1291-1338. [DOI:10.1007/978-3-030-88832-9_30]
8. Dispenza F, De Stefano A. Textbook of vertigo: Diagnosis and management. International Tinnitus Journal. 2012;17(2):111. [DOI:10.5935/0946-5448.20120020] [PMID]
9. Dasgupta A, Shepard NT, Jacobson GP. Vestibular disorders in children: Clinical assessment and management. In: Jacobson GP, Shepard NT, editors. Disorders of the Vestibular System. Cham: Springer; 2023. p. 201-218. [DOI:10.1007/978-3-031-40524-2_11]
10. Shiozaki T, Okada Y, Nakamura J, Ueta K, Tanaka H, Moritani M, Kitahara T. Relationships between changes in lateral vestibulospinal tract excitability and postural control by dynamic balance intervention in healthy individuals: A preliminary study. Frontiers in Human Neuroscience. 2023;17:1109690. [DOI:10.3389/fnhum.2023.1109690] [PMID]
11. Agrawal Y, Smith PF, Rosenberg PB. Vestibular impairment, cognitive decline and Alzheimer's disease: Balancing the evidence. Aging and Mental Health. 2020;24(5):705-708. [DOI:10.1080/13607863.2019.1566813] [PMID]
12. Yesantharao LV, Rosenberg P, Oh E, Leoutsakos J, Munro CA, et al. Vestibular therapy to reduce falls in people with Alzheimer's disease: Study protocol for a pilot randomized controlled trial. Pilot and Feasibility Studies. 2022;8(1):167. [DOI:10.1186/s40814-022-01133-w] [PMID]
13. Salehi L, Akhondzadeh E, Esmaelzadeh Saeieh S, Yazd Khasti M. The fall risk assessment and correlated factors among Iranians' older adults. Working with Older People. 2019;23(1):27-36. [DOI:10.1108/WWOP-11-2018-0020]
14. Borhaninejad V, Rashedi V, Tabe R, Delbari A, Ghasemzadeh H. Relationship between fear of falling and physical activity in older adults. Medical Journal of Mashhad University of Medical Sciences. 2015;58(8):446-452.
15. Daneshmandi H. The effect of virtual reality training program on the functional fitness of the elderly. Journal of Gerontology. 2021;6(1):32-41.
16. Bogle JM, Benarroch E, Sandroni P. Vestibular-autonomic interactions: Beyond orthostatic dizziness. Current Opinion in Neurology. 2022;35(1):126-134. [DOI:10.1097/WCO.0000000000001013] [PMID]
17. Brown AM, Zifchock RA, Hillstrom HJ. The effects of limb dominance and fatigue on running biomechanics. Gait and Posture. 2014;39(3):915-919. [DOI:10.1016/j.gaitpost.2013.12.007] [PMID]
18. Sarvestan J, Kováčiková Z, Linduška P, Gonosová Z, Svoboda Z. Age-related effects on lower extremities muscular strength, sit-to-stand, and functional reaching tests among community-dwelling elderly females. Journal of Physical Education and Sport. 2020;20(6):3391-3399.
19. Promsri A. Neuromuscular control in incline and decline treadmill running: Insights into movement synergies for training and rehabilitation. Signals. 2025;6(1):2. [DOI:10.3390/signals6010002]
20. Promsri A. Neuromuscular control in postural stability: Insights into myoelectric activity involved in postural sway during bipedal balance tasks. Signals. 2025;6(1):6. [DOI:10.3390/signals6010006]
21. Wang J, Li Y, Yang GY, Jin K. Age-related dysfunction in balance: A comprehensive review of causes, consequences, and interventions. Aging and Disease. 2024;16(2):714. [DOI:10.14336/AD.2024.0124-1] [PMID]
22. Van Hecke R, Danneels M, Dhooge I, Van Waelvelde H, Wiersema JR, Deconinck FJ, Maes L. Vestibular function in children with neurodevelopmental disorders: A systematic review. Journal of Autism and Developmental Disorders. 2019;49(8):3328-3350. [DOI:10.1007/s10803-019-04059-0] [PMID]
23. Gurberg J, Traboulsi H, Brodsky JR. Balance and vestibular disorders in children and adolescents. In: Jacobson GP, Shepard NT, editors. Disorders of the Vestibular System: Diagnosis and Management. Cham: Springer International Publishing; 2023. p. 179-199. [DOI:10.1007/978-3-031-40524-2_10]
24. Magnani RM, van Dieën JH, Bruijn SM. Effects of vestibular stimulation on gait stability when walking at different step widths. Experimental Brain Research. 2023;241(1):49-58. [DOI:10.1007/s00221-022-06488-3] [PMID]
25. Kozieł SM, Malina RM. Modified maturity offset prediction equations: Validation in independent longitudinal samples of boys and girls. Sports Medicine. 2018;48:221-236. [DOI:10.1007/s40279-017-0750-y] [PMID]
26. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39(2):175-191. [DOI:10.3758/BF03193146] [PMID]
27. Horak FB, Macpherson JM. Postural orientation and equilibrium. In: Handbook of Physiology. Section 12: Exercise: Regulation and Integration of Multiple Systems. Bethesda: American Physiological Society; 2016. p. 255-292. [DOI:10.1002/cphy.cp120107]
28. Herssens N, McCrum C. Stimulating balance: Recent advances in vestibular stimulation for balance and gait. Journal of Neurophysiology. 2019;122(2):563-576. [DOI:10.1152/jn.00851.2018] [PMID]
29. Paul M, Biswas SK, Sandhu JS. Role of sports vision and eye hand coordination training in performance of table tennis players. Brazilian Journal of Biomotricity. 2011;5(2):106-116.
30. A'ali Sh RF. Comparison of physical fitness of blind and deaf children with normal peers. Sport Medicine Studies. 2015;5(14):135-150.
31. Coello-Villalón M, López-Muñoz P, Palomo-Carrión R, Hidalgo-Robles Á, Merino-Andrés J. Short-term effects of vestibular training on gross motor function in children and youth with cerebral palsy: A systematic review and meta-analysis of randomized clinical trials. Physical and Occupational Therapy in Pediatrics. 2024;44(5):615-625. [DOI:10.1080/01942638.2024.2350385] [PMID]
32. Mitsutake T, Taniguchi T, Nakazono H, Yoshizuka H, Sakamoto M. Effects of noisy galvanic vestibular stimulation on the muscle activity and joint movements in different standing postures conditions. Frontiers in Human Neuroscience. 2022;16:891669. [DOI:10.3389/fnhum.2022.891669] [PMID]
33. Božanić Urbančič M, Novak A, Kovač M. Vestibular stimulation and motor development in children: A review. Child Development Research. 2024;2024:1-10.
34. Subramaniyam A, Rajendran R, Rajeswari R. Effectiveness of vestibular stimulation and neuromuscular exercise on balance in Down syndrome. International Journal of Childhood Development Disorders. 2024;5(1):20-24.
35. Eslami A, Sahebozamani M, Bahiraei S. The effect of the FIFA 11+ kids warm-up training program on lower limb injury prevention and football player performance: A systematic review. Journal of Sport Biomechanics. 2023;9(1):2-15. [DOI:10.61186/JSportBiomech.9.1.2]
36. Wuehr M, Nusser E, Krafczyk S, Straube A, Brandt T, Jahn K, Schniepp R. Noise-enhanced vestibular input improves dynamic walking stability in healthy subjects. Brain Stimulation. 2016;9(1):109-116. [DOI:10.1016/j.brs.2015.08.017] [PMID]
37. Fujimoto C, Yamamoto Y, Kamogashira T, Kinoshita M, Iwasaki S. Vestibular dysfunction does not significantly alter lower limb muscle activation during quiet standing. Journal of Neurophysiology. 2018;119(6):2145-2152.
38. Marchand S, Langlade A, Legois Q, Séverac Cauquil A. A wide-ranging review of galvanic vestibular stimulation: From its genesis to basic science and clinical applications. Experimental Brain Research. 2025;243(5):1-31. [DOI:10.1007/s00221-025-07079-8] [PMID]
39. Roshan S, Souri R, Jalilvand M. Effectiveness of a Kata exercise course on static and dynamic balance in hyperactive children. Journal of Sport Biomechanics. 2024;9(4):272-283. [DOI:10.61186/JSportBiomech.9.4.272]
40. Goldberg EJ, Neptune RR. Compensatory strategies during normal walking in response to muscle weakness and increased hip joint stiffness. Gait and Posture. 2007;25(3):360-367. [DOI:10.1016/j.gaitpost.2006.04.009] [PMID]
41. Biju K, Oh E, Rosenberg P, Xue QL, Dash P, et al. Vestibular function predicts balance and fall risk in patients with Alzheimer's disease. Journal of Alzheimer's Disease. 2022;86(3):1159-1168. [DOI:10.3233/JAD-215366] [PMID]
42. Ning S, Jorfi M, Patel SR, Kim DY, Tanzi RE. Neurotechnological approaches to the diagnosis and treatment of Alzheimer's disease. Frontiers in Neuroscience. 2022;16:854992. [DOI:10.3389/fnins.2022.854992] [PMID]
43. Smith PF. Hearing loss versus vestibular loss as contributors to cognitive dysfunction. Journal of Neurology. 2022;269(1):87-99. [DOI:10.1007/s00415-020-10343-2] [PMID]
44. Coughlan G, Plumb W, Zhukovsky P, Aung MH, Hornberger M. Vestibular contribution to path integration deficits in 'at-genetic-risk' for Alzheimer's disease. PLoS ONE. 2023;18(1):e0278239. [DOI:10.1371/journal.pone.0278239] [PMID]
45. Alyarnezhad CH, Daneshmandi H, Samami N. The comparison of upper cross syndrome in children with visual and hearing impairments with normal counterparts. Research in Sport Medicine and Technology. 2018;16(15):57-65.
46. Chepisheva MK. Spatial orientation, postural control and the vestibular system in healthy elderly and Alzheimer's dementia. PeerJ. 2023;11:e15040. [DOI:10.7717/peerj.15040] [PMID]
47. Plaza-Florido A, Pérez-Prieto I, Molina-Garcia P, Radom-Aizik S, Ortega FB, et al. Transcriptional and epigenetic response to sedentary behavior and physical activity in children and adolescents: A systematic review. Frontiers in Pediatrics. 2022;10:917152. [DOI:10.3389/fped.2022.917152]
48. Mucci V, Hamid M, Jacquemyn Y, Browne CJ. Influence of sex hormones on vestibular disorders. Current Opinion in Neurology. 2022;35(1):135-141. [DOI:10.1097/WCO.0000000000001019] [PMID]
49. Tramontano M, Martino C, Cerritelli F, et al. Vestibular rehabilitation in traumatic brain injury: A systematic review. Sensors. 2022;22(21):8553. [DOI:10.3390/s22218553] [PMID]
50. Meng L, Wang Y, Zhang H, et al. Vestibular rehabilitation therapy on balance and gait after stroke: A systematic review and meta-analysis. BMC Medicine. 2023;21(1):322. [DOI:10.1186/s12916-023-03029-9] [PMID]
51. Fan S, Zhang Y, Liu H, et al. Perturbation training and hip unloading strategies in stroke rehabilitation. Frontiers in Neurology. 2025;16:112345. [DOI:10.3389/fneur.2025.1495071] [PMID]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








