Volume 10, Issue 4 (1-2025)
J Sport Biomech 2025, 10(4): 294-308 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Azadian E, Jabar Ali M. The Relationship between Executive Functions and Postural Control in Children with Mild Intellectual Disability and Comparison with Typically Developing Peers. J Sport Biomech 2025; 10 (4) :294-308
URL: http://biomechanics.iauh.ac.ir/article-1-359-en.html
URL: http://biomechanics.iauh.ac.ir/article-1-359-en.html
1- Department of Motor Behavior, Hamedan Branch, Islamic Azad University, Hamedan, Iran.
2- Physical Education and Sport Sciences Department, University of Halabja, Halabja, Kurdistan Region, Iraq.
2- Physical Education and Sport Sciences Department, University of Halabja, Halabja, Kurdistan Region, Iraq.
Keywords: Executive functions, Postural control, Children with intellectual disability, Center of pressure, Static
Full-Text [PDF 1890 kb]
(901 Downloads)
| Abstract (HTML) (2492 Views)
Full-Text: (1347 Views)
Extended Abstract
1. Introduction
Children with intellectual disabilities (ID) experience significant challenges in both cognitive and motor functions, which greatly affect their daily lives (2). These challenges often show up as difficulties in maintaining balance and postural control, both of which are essential for carrying out everyday tasks and ensuring physical safety (15,16). Postural control is a complex process that requires the integration of sensory information and motor responses. This process is especially impaired in children with ID due to issues with sensory processing and motor planning (17.18). Executive functions (EF)—which include cognitive skills like attention, working memory, inhibitory control, and cognitive flexibility—are critical for maintaining balance, especially in dynamic environments (3). Previous studies have highlighted the link between EF and motor performance (25). However, there is limited research examining the specific interaction between EF and postural control in this group. This study aims to explore the relationship between EF and postural control in children with ID and compare their performance with that of typically developing (TD) children. The results are expected to offer insights into the underlying causes of postural instability in children with ID and help guide the development of targeted interventions..
2. Methods
This causal-comparative and correlational study involved 15 individuals with ID and 15 TD as the control group. Participants were recruited from special education and mainstream schools, respectively. The inclusion criteria for both groups included being within the age range of 7–12 years. Exclusion criteria included the presence of neurological disorders (other than ID in the ID group), chronic medical conditions, visual impairments, or physical disabilities affecting balance.
Static balance was assessed using a force plate (Kistler 9281 EA) under two conditions: stable (barefoot on the force plate) and unstable (standing on foam placed on the force plate). Center of pressure (CoP) parameters, including sway, speed, and displacement in the anterior-posterior (AP) and medial-lateral (ML) directions, were recorded. Executive functions (EF) were assessed using simple reaction time and response inhibition (Go/No Go) tests.
The Shapiro-Wilk test was used to assess data normality. Since the balance data followed a normal distribution, a three-way repeated measures ANOVA was conducted for between-group comparisons of balance variables. As the cognitive data were not normally distributed, the Mann-Whitney U test was used for group comparisons of cognitive performance. Spearman’s correlation coefficient was used to examine the relationship between balance performance (CoP sway) and cognitive performance (reaction time and response inhibition). Statistical significance was set at p < 0.05.
3. Results
The results showed significant differences between the ID and TD groups in both cognitive and postural control measures. Children with ID had slower reaction times and higher rates of incorrect responses on the cognitive tests compared to TD children (p < 0.05). Regarding postural control, children with ID exhibited greater sway, faster speed, and increased variability in both the AP and ML directions, especially under unstable conditions (p < 0.05) (Table 1). The interaction between task type (stable vs. unstable) and direction (AP vs. ML) was significant for CoP speed, with the ID group showing a notable increase in ML speed during unstable conditions (p < 0.05).
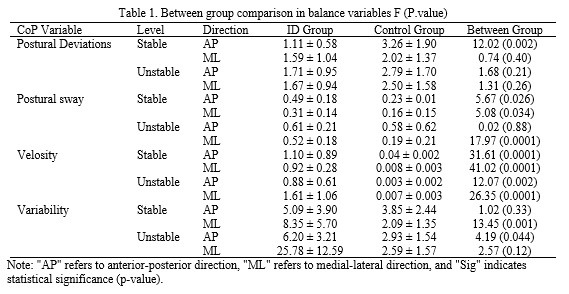
Correlation analyses revealed strong to moderate relationships between cognitive performance and postural control variables. Specifically, the number of unresponsive stimuli in the reaction time test was positively correlated with CoP speed and variability in the AP direction under stable conditions, as well as with postural deviations, sway, and speed in the ML direction under unstable conditions (r = 0.51–0.66). On the other hand, the number of correct responses was negatively correlated with CoP speed and variability in the AP direction (r = -0.82 and -0.56, respectively). These findings suggest that deficits in attention and processing speed may contribute to postural instability in children with ID.
4. Conclusion
The findings of this study highlight the significant impact of ID on both cognitive and motor functions. Children with ID demonstrated slower reaction times and higher error rates in cognitive tasks, which aligns with previous research pointing to deficits in EF within this population. These cognitive impairments are likely contributing factors to the observed postural instability, as EF are crucial for integrating sensory inputs and generating appropriate motor responses (33). The increased CoP sway and speed observed in children with ID, especially under unstable conditions, may suggest the use of compensatory strategies to maintain balance. However, these strategies appear to be less efficient and more energy-consuming, possibly leading to greater fatigue and an increased risk of falls (39). The strong correlations between cognitive performance and postural control measures underscore the importance of EF in maintaining balance. Specifically, deficits in attention and inhibitory control may hinder the ability of children with ID to effectively adapt to dynamic postural challenges, resulting in greater instability (36). These findings are consistent with previous studies that suggest EF and postural control share overlapping neural substrates, such as the prefrontal cortex and cerebellum.
The study also emphasizes the need to address both cognitive and motor deficits in interventions for children with ID (27,36). Comprehensive programs that combine cognitive-motor training, balance exercises, and strength training could be beneficial in improving postural control and reducing the risk of falls in this population. Finally, future research should delve deeper into the neural mechanisms underlying the relationship between EF and postural control in children with ID, and assess the long-term effectiveness of targeted interventions in enhancing both cognitive and motor outcomes.
This study provides compelling evidence of the significant impact of ID on both cognitive processing and postural control. Children with ID exhibit slower reaction times, higher error rates, and greater postural instability compared to TD children, particularly under more challenging conditions. The increased CoP speed and variability observed in children with ID may indicate the use of inefficient compensatory strategies to maintain balance, which could lead to increased fatigue and a higher risk of falls. The strong correlations between cognitive performance and postural control variables emphasize the critical role of EF in maintaining balance. These findings underscore the importance of integrated interventions that address both cognitive and motor deficits in children with ID. Future research should focus on developing and evaluating targeted interventions that not only aim to improve postural control but also enhance overall quality of life for children with intellectual disabilities.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be addressed in this research.
Funding
This research did not receive any financial support from government, private, or non-profit organizations.
Authors' contributions
All authors contributed equally to preparing the article.
Conflicts of interest
The authors declare that there are no conflicts of interest associated with this article.
Children with intellectual disabilities (ID) experience significant challenges in both cognitive and motor functions, which greatly affect their daily lives (2). These challenges often show up as difficulties in maintaining balance and postural control, both of which are essential for carrying out everyday tasks and ensuring physical safety (15,16). Postural control is a complex process that requires the integration of sensory information and motor responses. This process is especially impaired in children with ID due to issues with sensory processing and motor planning (17.18). Executive functions (EF)—which include cognitive skills like attention, working memory, inhibitory control, and cognitive flexibility—are critical for maintaining balance, especially in dynamic environments (3). Previous studies have highlighted the link between EF and motor performance (25). However, there is limited research examining the specific interaction between EF and postural control in this group. This study aims to explore the relationship between EF and postural control in children with ID and compare their performance with that of typically developing (TD) children. The results are expected to offer insights into the underlying causes of postural instability in children with ID and help guide the development of targeted interventions..
2. Methods
This causal-comparative and correlational study involved 15 individuals with ID and 15 TD as the control group. Participants were recruited from special education and mainstream schools, respectively. The inclusion criteria for both groups included being within the age range of 7–12 years. Exclusion criteria included the presence of neurological disorders (other than ID in the ID group), chronic medical conditions, visual impairments, or physical disabilities affecting balance.
Static balance was assessed using a force plate (Kistler 9281 EA) under two conditions: stable (barefoot on the force plate) and unstable (standing on foam placed on the force plate). Center of pressure (CoP) parameters, including sway, speed, and displacement in the anterior-posterior (AP) and medial-lateral (ML) directions, were recorded. Executive functions (EF) were assessed using simple reaction time and response inhibition (Go/No Go) tests.
The Shapiro-Wilk test was used to assess data normality. Since the balance data followed a normal distribution, a three-way repeated measures ANOVA was conducted for between-group comparisons of balance variables. As the cognitive data were not normally distributed, the Mann-Whitney U test was used for group comparisons of cognitive performance. Spearman’s correlation coefficient was used to examine the relationship between balance performance (CoP sway) and cognitive performance (reaction time and response inhibition). Statistical significance was set at p < 0.05.
3. Results
The results showed significant differences between the ID and TD groups in both cognitive and postural control measures. Children with ID had slower reaction times and higher rates of incorrect responses on the cognitive tests compared to TD children (p < 0.05). Regarding postural control, children with ID exhibited greater sway, faster speed, and increased variability in both the AP and ML directions, especially under unstable conditions (p < 0.05) (Table 1). The interaction between task type (stable vs. unstable) and direction (AP vs. ML) was significant for CoP speed, with the ID group showing a notable increase in ML speed during unstable conditions (p < 0.05).
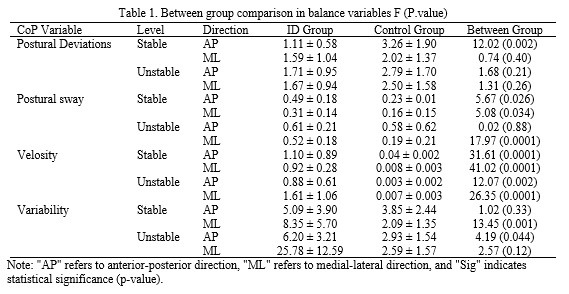
Correlation analyses revealed strong to moderate relationships between cognitive performance and postural control variables. Specifically, the number of unresponsive stimuli in the reaction time test was positively correlated with CoP speed and variability in the AP direction under stable conditions, as well as with postural deviations, sway, and speed in the ML direction under unstable conditions (r = 0.51–0.66). On the other hand, the number of correct responses was negatively correlated with CoP speed and variability in the AP direction (r = -0.82 and -0.56, respectively). These findings suggest that deficits in attention and processing speed may contribute to postural instability in children with ID.
4. Conclusion
The findings of this study highlight the significant impact of ID on both cognitive and motor functions. Children with ID demonstrated slower reaction times and higher error rates in cognitive tasks, which aligns with previous research pointing to deficits in EF within this population. These cognitive impairments are likely contributing factors to the observed postural instability, as EF are crucial for integrating sensory inputs and generating appropriate motor responses (33). The increased CoP sway and speed observed in children with ID, especially under unstable conditions, may suggest the use of compensatory strategies to maintain balance. However, these strategies appear to be less efficient and more energy-consuming, possibly leading to greater fatigue and an increased risk of falls (39). The strong correlations between cognitive performance and postural control measures underscore the importance of EF in maintaining balance. Specifically, deficits in attention and inhibitory control may hinder the ability of children with ID to effectively adapt to dynamic postural challenges, resulting in greater instability (36). These findings are consistent with previous studies that suggest EF and postural control share overlapping neural substrates, such as the prefrontal cortex and cerebellum.
The study also emphasizes the need to address both cognitive and motor deficits in interventions for children with ID (27,36). Comprehensive programs that combine cognitive-motor training, balance exercises, and strength training could be beneficial in improving postural control and reducing the risk of falls in this population. Finally, future research should delve deeper into the neural mechanisms underlying the relationship between EF and postural control in children with ID, and assess the long-term effectiveness of targeted interventions in enhancing both cognitive and motor outcomes.
This study provides compelling evidence of the significant impact of ID on both cognitive processing and postural control. Children with ID exhibit slower reaction times, higher error rates, and greater postural instability compared to TD children, particularly under more challenging conditions. The increased CoP speed and variability observed in children with ID may indicate the use of inefficient compensatory strategies to maintain balance, which could lead to increased fatigue and a higher risk of falls. The strong correlations between cognitive performance and postural control variables emphasize the critical role of EF in maintaining balance. These findings underscore the importance of integrated interventions that address both cognitive and motor deficits in children with ID. Future research should focus on developing and evaluating targeted interventions that not only aim to improve postural control but also enhance overall quality of life for children with intellectual disabilities.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be addressed in this research.
Funding
This research did not receive any financial support from government, private, or non-profit organizations.
Authors' contributions
All authors contributed equally to preparing the article.
Conflicts of interest
The authors declare that there are no conflicts of interest associated with this article.
Type of Study: Research |
Subject:
Special
Received: 2025/02/3 | Accepted: 2025/02/12 | Published: 2025/02/13
Received: 2025/02/3 | Accepted: 2025/02/12 | Published: 2025/02/13
References
1. Fragkou D, Gkrimas G, Pyrgeli M. Therapeutic interventions for trunk and improvement of posture in children with cerebral palsy: A review of the literature. MOJ Orthop Rheumatol. 2018;10(4):288-96. [DOI:10.15406/mojor.2018.10.00434]
2. Robertson J, Baines S, Emerson E, Hatton C. Postural care for people with intellectual disabilities and severely impaired motor function: A scoping review. Journal of applied research in intellectual disabilities. 2018;31:11-28. [DOI:10.1111/jar.12325] [PMID]
3. Chen Y, Yu Y, Niu R, Liu Y. Selective Effects of Postural Control on Spatial vs. Nonspatial Working Memory: A Functional Near-Infrared Spectral Imaging Study. Front Hum Neurosci. 2018; 12 (June): 1-11. [DOI:10.3389/fnhum.2018.00243] [PMID]
4. Hartman E, Houwen S, Scherder E, Visscher C. On the relationship between motor performance and executive functioning in children with intellectual disabilities. Journal of Intellectual Disability Research. 2010;54(5):468-77. [DOI:10.1111/j.1365-2788.2010.01284.x] [PMID]
5. Friedman NP, Miyake A, Corley RP, Young SE, DeFries JC, Hewitt JK. Not all executive functions are related to intelligence. Psychological science. 2006;17(2):172-9. [DOI:10.1111/j.1467-9280.2006.01681.x] [PMID]
6. Chevalère J, Postal V, Jauregui J, Copet P, Laurier V, Thuilleaux D. Assessment of Executive Functions in P rader-W illi Syndrome and Relationship with Intellectual Level. Journal of Applied Research in Intellectual Disabilities. 2013;26(4):309-18. [DOI:10.1111/jar.12044] [PMID]
7. Costanzo F, Varuzza C, Menghini D, Addona F, Gianesini T, Vicari S. Executive functions in intellectual disabilities: a comparison between Williams syndrome and Down syndrome. Research in developmental disabilities. 2013;34(5):1770-80. [DOI:10.1016/j.ridd.2013.01.024] [PMID]
8. Happé F, Booth R, Charlton R, Hughes C. Executive function deficits in autism spectrum disorders and attention-deficit/hyperactivity disorder: examining profiles across domains and ages. Brain and cognition. 2006;61(1):25-39. [DOI:10.1016/j.bandc.2006.03.004] [PMID]
9. Wilding J, Cornish K, Munir F. Further delineation of the executive deficit in males with fragile-X syndrome. Neuropsychologia. 2002;40(8):1343-9. [DOI:10.1016/S0028-3932(01)00212-3] [PMID]
10. Woodcock KA, Oliver C, Humphreys GW. Task-switching deficits and repetitive behaviour in genetic neurodevelopmental disorders: Data from children with Prader-Willi syndrome chromosome 15 q11-q13 deletion and boys with Fragile X syndrome. Cognitive Neuropsychology. 2009;26(2):172-94. [DOI:10.1080/02643290802685921] [PMID]
11. Kranzler JH, Jensen AR. Inspection time and intelligence: A meta-analysis. Intelligence. 1989;13(4):329-47. [DOI:10.1016/S0160-2896(89)80006-6]
12. Lipowicz A, Bugdol MN, Szurmik T, Bibrowicz K, Kurzeja P, Mitas AW. Body balance analysis of children and youth with intellectual disabilities. Journal of Intellectual Disability Research. 2019;63(11):1312-23. [DOI:10.1111/jir.12671] [PMID]
13. Azadian E, Nasab AD, Majlesi M, Rezaie M. Effect of manipulation of base of support on center of pressure: comparison of children with and without intellectual disability. Kinesiologia Slovenica: scientific journal on sport. 2023;29(3):75-86. [DOI:10.52165/kinsi.29.3.75-86]
14. Dehghan Nasab A, Azadian E. Relationship between Fundamental Movement Skills and Variability in Postural Control: Comparison of Children with and without Intellectual Disability. Pajouhan Scientific Journal. 2024;22(1):31-41. [DOI:10.61186/psj.22.1.31]
15. Yu C, Li J, Liu Y, Qin W, Li Y, Shu N, et al. White matter tract integrity and intelligence in patients with mental retardation and healthy adults. Neuroimage. 2008;40(4):1533-41. [DOI:10.1016/j.neuroimage.2008.01.063] [PMID]
16. Hall JM, Thomas MJ. Promoting physical activity and exercise in older adults with developmental disabilities. Topics in Geriatric Rehabilitation. 2008;24(1):64-73. [DOI:10.1097/01.TGR.0000311407.09178.55]
17. Kachouri H, Jouira G, Laatar R, Borji R, Rebai H, Sahli S. Different types of combined training programs to improve postural balance in single and dual tasks in children with intellectual disability. Journal of Intellectual Disabilities. 2024;28(1):225-39. [DOI:10.1177/17446295221148585] [PMID]
18. Ho P, Bulsara M, Patman S, Downs J, Bulsara C, Hill AM. Incidence and associated risk factors for falls in adults with intellectual disability. Journal of Intellectual Disability Research. 2019;63(12):1441-52. [DOI:10.1111/jir.12686] [PMID]
19. Pal J, Hale L, Mirfin-Veitch B, Claydon L. Injuries and falls among adults with intellectual disability: A prospective New Zealand cohort study. Journal of Intellectual and Developmental Disability. 2014;39(1):35-44. [DOI:10.3109/13668250.2013.867929]
20. Hsieh K, Rimmer J, Heller T. Prevalence of falls and risk factors in adults with intellectual disability. American journal on intellectual and developmental disabilities. 2012;117(6):442-54. [DOI:10.1352/1944-7558-117.6.442] [PMID]
21. Bibrowicz K, Szurmik T, Wodarski P, Michnik R, Mysliwiec A, Barszcz J, et al. Quality of body posture and postural stability in people with intellectual disability playing volleyball. Acta of Bioengineering and Biomechanics. 2019;21(1):23-30.
22. Lipsitz LA, Goldberger AL. Loss of'complexity'and aging: potential applications of fractals and chaos theory to senescence. Jama. 1992;267(13):1806-9. [DOI:10.1001/jama.1992.03480130122036]
23. Stergiou N, Yu Y, Kyvelidou A. A perspective on human movement variability with applications in infancy motor development. Kinesiology Review. 2013;2(1):93-102. [DOI:10.1123/krj.2.1.93]
24. Stergiou N, Decker LM. Human movement variability, nonlinear dynamics, and pathology: is there a connection? Human movement science. 2011;30(5):869-88. [DOI:10.1016/j.humov.2011.06.002] [PMID]
25. Suarez LV. Relationship Between Executive Function and Postural Control. 2019.
26. Chen Y, Yu Y, Niu R, Liu Y. Selective effects of postural control on spatial vs. nonspatial working memory: A functional near-infrared spectral imaging study. Frontiers in human neuroscience. 2018;12:243. [DOI:10.3389/fnhum.2018.00243] [PMID]
27. Koziol LF, Budding DE, Chidekel D. From movement to thought: executive function, embodied cognition, and the cerebellum. The Cerebellum. 2012;11(2):505-25. [DOI:10.1007/s12311-011-0321-y] [PMID]
28. Rocchi L, Chiari L, Horak F. Effects of deep brain stimulation and levodopa on postural sway in Parkinson's disease. Journal of Neurology, Neurosurgery & Psychiatry. 2002;73(3):267-74. [DOI:10.1136/jnnp.73.3.267] [PMID]
29. Wodka EL, Mark Mahone E, Blankner JG, Gidley Larson JC, Fotedar S, Denckla MB, et al. Evidence that response inhibition is a primary deficit in ADHD. Journal of clinical and experimental neuropsychology. 2007;29(4):345-56. [DOI:10.1080/13803390600678046] [PMID]
30. Schuchardt K, Maehler C, Hasselhorn M. Working memory deficits in children with specific learning disorders. Journal of learning Disabilities. 2008;41(6):514-23. [DOI:10.1177/0022219408317856] [PMID]
31. Van der Molen MJ, Van Luit JE, Jongmans MJ, Van der Molen MW. Verbal working memory in children with mild intellectual disabilities. Journal of Intellectual Disability Research. 2007;51(2):162-9. [DOI:10.1111/j.1365-2788.2006.00863.x] [PMID]
32. Doherty MJ, Campbell NM, Tsuji H, Phillips WA. The Ebbinghaus illusion deceives adults but not young children. Developmental science. 2010;13(5):714-21. [DOI:10.1111/j.1467-7687.2009.00931.x] [PMID]
33. Diamond A. Executive functions. Annual review of psychology. 2013;64(1):135-68. [DOI:10.1146/annurev-psych-113011-143750] [PMID]
34. Vuijk PJ, Hartman E, Scherder E, Visscher C. Motor performance of children with mild intellectual disability and borderline intellectual functioning. Journal of intellectual disability research. 2010;54(11):955-65. [DOI:10.1111/j.1365-2788.2010.01318.x] [PMID]
35. Shumway-Cook A. Motor control: Translating research into clinical practice. Lippincoot Williams & Wilkins. 2007.
36. Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age and ageing. 2006;35(suppl_2):ii7-ii11. [DOI:10.1093/ageing/afl077] [PMID]
37. Winter DA, Patla AE, Prince F, Ishac M, Gielo-Perczak K. Stiffness control of balance in quiet standing. Journal of neurophysiology. 1998;80(3):1211-21. [DOI:10.1152/jn.1998.80.3.1211] [PMID]
38. Azimizadeh MJ, Hoseini SH, Norasteh AA. Effect of a Combined Strengthening and Proprioceptive Training Program on Balance and Gait of Female Children With Intellectual Disability. Journal of Sport Biomechanics. 2021;7(2):136-47. [DOI:10.32598/biomechanics.7.2.5]
39. Hale JB, Reddy LA, Semrud-Clikeman M, Hain LA, Whitaker J, Morley J, et al. Executive impairment determines ADHD medication response: implications for academic achievement. Journal of Learning Disabilities. 2011;44(2):196-212. [DOI:10.1177/0022219410391191] [PMID]
40. Woollacott M, Shumway-Cook A. Attention and the control of posture and gait: a review of an emerging area of research. Gait & posture. 2002;16(1):1-14. [DOI:10.1016/S0966-6362(01)00156-4] [PMID]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |