Volume 11, Issue 1 (6-2025)
J Sport Biomech 2025, 11(1): 2-19 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadi Yaghoubi U, Farahpour N, Mansoorizadeh M, Moisan G. Evaluation of Single-leg Balance during Landing from 20- and 40-centimeter Heights in Individuals with and without Chronic Ankle Instability. J Sport Biomech 2025; 11 (1) :2-19
URL: http://biomechanics.iauh.ac.ir/article-1-362-en.html
URL: http://biomechanics.iauh.ac.ir/article-1-362-en.html
1- Department of Sport Biomechanics, Faculty of Sport Sciences, Bu-Ali Sina University, Hamedan, Iran.
2- Department of Computer Engineering, Bu-Ali Sina University, Hamedan, Iran.
3- Department of Human Kinetics, Université du Québec à Trois-Rivières, Québec, Canada.
2- Department of Computer Engineering, Bu-Ali Sina University, Hamedan, Iran.
3- Department of Human Kinetics, Université du Québec à Trois-Rivières, Québec, Canada.
Full-Text [PDF 1726 kb]
(815 Downloads)
| Abstract (HTML) (3198 Views)
Full-Text: (1276 Views)
Extended Abstract
1. Introduction
Ankle sprains are among the most common injuries, particularly in athletes, with up to 67% associated with high-impact mechanisms (3). These injuries typically result from sudden supination or inversion during transitions between weight-bearing and non-weight-bearing phases, leading to strain in ligaments such as the anterior talofibular and calcaneofibular ligaments (4, 5). Studies indicate that approximately 32% to 74% of individuals with severe sprains go on to develop chronic ankle instability (CAI), characterized by symptoms such as giving way and recurrent sprains (6). CAI is linked to balance deficits stemming from muscle weakness, impaired neuromuscular control, and joint stiffness (8, 9, 10). Recent research has shown that individuals with CAI exhibit increased center of pressure (COP) displacement and velocity during balance tasks compared to healthy controls (19). Fatigue further exacerbates these differences, significantly affecting COP-related parameters in the CAI population (20). Moreover, asymmetries in COP movement patterns have been reported between injured and uninjured limbs during landing tasks (21, 22). Despite these findings, much of the existing research has focused on relatively simple balance tasks, highlighting the need to investigate more demanding conditions—such as landings from different heights. Therefore, the present study aims to evaluate balance performance by analyzing COP kinematics during single-leg landings from 20 and 40 centimeters in individuals with CAI, compared to healthy controls. We hypothesize that individuals with CAI will exhibit greater COP fluctuations and that increased landing height will exacerbate balance deficits. These insights may contribute to a better understanding of injury mechanisms and inform more effective rehabilitation strategies.
2. Methods
In this study, 17 individuals with chronic ankle instability were included as the experimental group, and 17 healthy individuals served as the control group. All participants were between 20 and 40 years old and were physically active. Members of the experimental group were recruited through orthopedic clinics in the city, sports clubs, poster announcements at universities and sports centers, and advertisements on social media. The ankle injuries in the experimental group were non-contact in nature.
The study measured COP variables using a Kistler force plate (Kistler AG, Winterthur, Switzerland) with dimensions of 40 × 60 cm, capturing force data at a sampling rate of 1000 Hz. The force plate was calibrated with the axes oriented laterally (X), anteriorly (Y), and vertically upward (Z). For the landing tasks from heights of 20 cm and 40 cm, wooden platforms were positioned 5 cm away from the edge of the force plate. Participants performed two movement tasks: four single-leg landings from each height, resulting in a total of eight randomized trials. Prior to the main trials, all participants completed a 5-minute warm-up in the laboratory, which included practice landings. For the single-leg landing task, participants stood barefoot on the platform with their non-dominant leg raised and hands placed on their hips to minimize upper limb movement. At the auditory cue "go," participants executed the landing on the force plate and maintained a single-leg stance for 10 seconds without moving their foot (26). Trials were repeated if the participant lost balance during landing or failed to maintain the stance for the full 10 seconds. Data were initially recorded using QTM software and subsequently processed in Visual 3D (C-Motion, Inc., MD, USA), applying a 4th-order Butterworth low-pass filter. MATLAB (R2021a) was used to compute COP path length, range of motion, average radial displacement, and COP sway area.
Statistical analyses were performed using SPSS version 27. The Shapiro-Wilk test assessed data normality. Multivariate analysis of variance (MANOVA) was used for between-group comparisons, while repeated-measures ANOVA was applied for within-group comparisons. Statistical significance was set at p < 0.05.
3. Results
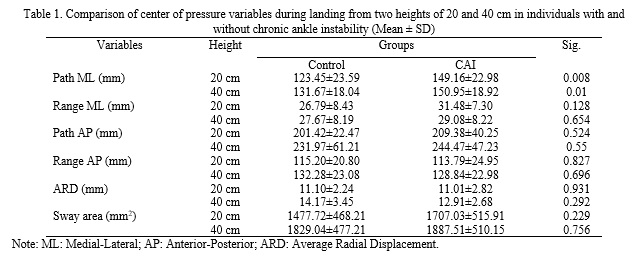
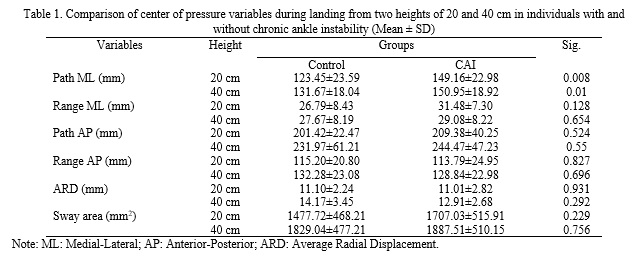
The results revealed significant differences between the experimental and control groups in medial-lateral COP path length during landings from both 20 cm (p = 0.008) and 40 cm (p = 0.01) heights (Table 1). Within-group comparisons indicated that, regardless of group, the range of COP motion in the anterior-posterior direction was approximately 4.2 times greater than that in the medial-lateral direction (p < 0.001). Increasing the landing height from 20 cm to 40 cm led to a 15% increase in anterior-posterior COP range (p < 0.001), whereas the medial-lateral range remained unaffected by the height change. Additionally, no significant between-group differences were observed in average radial displacement or COP sway area at either height (p > 0.05). However, within-group analyses showed that increasing height significantly influenced both variables: mean radial displacement increased by 27% (p < 0.001), and COP sway area increased by 22% (p = 0.015). In summary, although changes in landing height affected overall COP path and sway characteristics, they did not result in significant between-group differences in average radial displacement or sway area.
4. Conclusion
This study examined balance performance through COP kinematics during single-leg landings from 20 cm and 40 cm heights in individuals with and without CAI. The first hypothesis—that individuals with CAI would exhibit greater COP oscillations and displacements compared to healthy controls—was partially supported. Specifically, individuals with CAI demonstrated a significantly longer COP path in the medial-lateral (frontal plane) direction during landings, aligning with previous research. This finding suggests impaired postural control, likely stemming from deficits in proprioception and neuromuscular function caused by previous ankle sprains, which may damage joint receptors and muscle spindles.
Interestingly, while COP path length differed significantly between groups, the amplitude of COP oscillations in the frontal plane did not, implying that path length may be a more sensitive indicator of balance deficits in individuals with CAI. With increased landing height, both groups exhibited greater COP displacement—particularly in the anterior-posterior direction—likely due to elevated foot-ground impact forces and the increased neuromuscular demand required for shock absorption. Notably, both groups adapted similarly to the higher landing height, suggesting that CAI did not significantly alter this aspect of the biomechanical response. These findings underscore that individuals with CAI experience greater balance impairments, particularly in the frontal plane, during landing tasks. Furthermore, higher landing heights impose additional challenges to postural control, reinforcing the importance of targeted rehabilitation programs aimed at improving balance and reducing re-injury risk in this population.
Limitations of the study include the relatively small sample size, lack of control over participants’ activity levels, and the possibility of bias due to participants’ awareness of the landing task. Future research should explore the biomechanical deficits associated with CAI during more demanding functional tasks and develop evidence-based rehabilitation strategies to enhance postural stability and minimize injury recurrence.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be addressed in this research.
Funding
This research did not receive any financial support from government, private, or non-profit organizations.
Authors' contributions
All authors contributed equally to preparing the article.
Conflicts of interest
The authors declare that there are no conflicts of interest associated with this article.
Ankle sprains are among the most common injuries, particularly in athletes, with up to 67% associated with high-impact mechanisms (3). These injuries typically result from sudden supination or inversion during transitions between weight-bearing and non-weight-bearing phases, leading to strain in ligaments such as the anterior talofibular and calcaneofibular ligaments (4, 5). Studies indicate that approximately 32% to 74% of individuals with severe sprains go on to develop chronic ankle instability (CAI), characterized by symptoms such as giving way and recurrent sprains (6). CAI is linked to balance deficits stemming from muscle weakness, impaired neuromuscular control, and joint stiffness (8, 9, 10). Recent research has shown that individuals with CAI exhibit increased center of pressure (COP) displacement and velocity during balance tasks compared to healthy controls (19). Fatigue further exacerbates these differences, significantly affecting COP-related parameters in the CAI population (20). Moreover, asymmetries in COP movement patterns have been reported between injured and uninjured limbs during landing tasks (21, 22). Despite these findings, much of the existing research has focused on relatively simple balance tasks, highlighting the need to investigate more demanding conditions—such as landings from different heights. Therefore, the present study aims to evaluate balance performance by analyzing COP kinematics during single-leg landings from 20 and 40 centimeters in individuals with CAI, compared to healthy controls. We hypothesize that individuals with CAI will exhibit greater COP fluctuations and that increased landing height will exacerbate balance deficits. These insights may contribute to a better understanding of injury mechanisms and inform more effective rehabilitation strategies.
2. Methods
In this study, 17 individuals with chronic ankle instability were included as the experimental group, and 17 healthy individuals served as the control group. All participants were between 20 and 40 years old and were physically active. Members of the experimental group were recruited through orthopedic clinics in the city, sports clubs, poster announcements at universities and sports centers, and advertisements on social media. The ankle injuries in the experimental group were non-contact in nature.
The study measured COP variables using a Kistler force plate (Kistler AG, Winterthur, Switzerland) with dimensions of 40 × 60 cm, capturing force data at a sampling rate of 1000 Hz. The force plate was calibrated with the axes oriented laterally (X), anteriorly (Y), and vertically upward (Z). For the landing tasks from heights of 20 cm and 40 cm, wooden platforms were positioned 5 cm away from the edge of the force plate. Participants performed two movement tasks: four single-leg landings from each height, resulting in a total of eight randomized trials. Prior to the main trials, all participants completed a 5-minute warm-up in the laboratory, which included practice landings. For the single-leg landing task, participants stood barefoot on the platform with their non-dominant leg raised and hands placed on their hips to minimize upper limb movement. At the auditory cue "go," participants executed the landing on the force plate and maintained a single-leg stance for 10 seconds without moving their foot (26). Trials were repeated if the participant lost balance during landing or failed to maintain the stance for the full 10 seconds. Data were initially recorded using QTM software and subsequently processed in Visual 3D (C-Motion, Inc., MD, USA), applying a 4th-order Butterworth low-pass filter. MATLAB (R2021a) was used to compute COP path length, range of motion, average radial displacement, and COP sway area.
Statistical analyses were performed using SPSS version 27. The Shapiro-Wilk test assessed data normality. Multivariate analysis of variance (MANOVA) was used for between-group comparisons, while repeated-measures ANOVA was applied for within-group comparisons. Statistical significance was set at p < 0.05.
3. Results
The results revealed significant differences between the experimental and control groups in medial-lateral COP path length during landings from both 20 cm (p = 0.008) and 40 cm (p = 0.01) heights (Table 1). Within-group comparisons indicated that, regardless of group, the range of COP motion in the anterior-posterior direction was approximately 4.2 times greater than that in the medial-lateral direction (p < 0.001). Increasing the landing height from 20 cm to 40 cm led to a 15% increase in anterior-posterior COP range (p < 0.001), whereas the medial-lateral range remained unaffected by the height change. Additionally, no significant between-group differences were observed in average radial displacement or COP sway area at either height (p > 0.05). However, within-group analyses showed that increasing height significantly influenced both variables: mean radial displacement increased by 27% (p < 0.001), and COP sway area increased by 22% (p = 0.015). In summary, although changes in landing height affected overall COP path and sway characteristics, they did not result in significant between-group differences in average radial displacement or sway area.
4. Conclusion
This study examined balance performance through COP kinematics during single-leg landings from 20 cm and 40 cm heights in individuals with and without CAI. The first hypothesis—that individuals with CAI would exhibit greater COP oscillations and displacements compared to healthy controls—was partially supported. Specifically, individuals with CAI demonstrated a significantly longer COP path in the medial-lateral (frontal plane) direction during landings, aligning with previous research. This finding suggests impaired postural control, likely stemming from deficits in proprioception and neuromuscular function caused by previous ankle sprains, which may damage joint receptors and muscle spindles.
Interestingly, while COP path length differed significantly between groups, the amplitude of COP oscillations in the frontal plane did not, implying that path length may be a more sensitive indicator of balance deficits in individuals with CAI. With increased landing height, both groups exhibited greater COP displacement—particularly in the anterior-posterior direction—likely due to elevated foot-ground impact forces and the increased neuromuscular demand required for shock absorption. Notably, both groups adapted similarly to the higher landing height, suggesting that CAI did not significantly alter this aspect of the biomechanical response. These findings underscore that individuals with CAI experience greater balance impairments, particularly in the frontal plane, during landing tasks. Furthermore, higher landing heights impose additional challenges to postural control, reinforcing the importance of targeted rehabilitation programs aimed at improving balance and reducing re-injury risk in this population.
Limitations of the study include the relatively small sample size, lack of control over participants’ activity levels, and the possibility of bias due to participants’ awareness of the landing task. Future research should explore the biomechanical deficits associated with CAI during more demanding functional tasks and develop evidence-based rehabilitation strategies to enhance postural stability and minimize injury recurrence.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be addressed in this research.
Funding
This research did not receive any financial support from government, private, or non-profit organizations.
Authors' contributions
All authors contributed equally to preparing the article.
Conflicts of interest
The authors declare that there are no conflicts of interest associated with this article.
Type of Study: Research |
Subject:
Special
Received: 2025/02/15 | Accepted: 2025/02/28 | Published: 2025/04/3
Received: 2025/02/15 | Accepted: 2025/02/28 | Published: 2025/04/3
References
1. Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports medicine. 2014;44:123-140. [DOI:10.1007/s40279-013-0102-5] [PMID]
2. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont Jr PJ. The epidemiology of ankle sprains in the United States. Jbjs. 2010;92(13):2279-2284. [DOI:10.2106/JBJS.I.01537] [PMID]
3. Bagehorn T, de Zee M, Fong DT, Thorborg K, Kersting UG, Lysdal FG. Lateral ankle joint injuries in indoor and court sports: a systematic video analysis of 445 nonconsecutive case series. The American journal of sports medicine. 2024;52(6):1572-1584. [DOI:10.1177/03635465241241760] [PMID]
4. Delahunt E, Remus A. Risk factors for lateral ankle sprains and chronic ankle instability. Journal of athletic training. 2019;54(6):611-616. [DOI:10.4085/1062-6050-44-18] [PMID]
5. van den Bekerom MP, Kerkhoffs GM, McCollum GA, Calder JD, van Dijk CN. Management of acute lateral ankle ligament injury in the athlete. Knee surgery, sports traumatology, arthroscopy. 2013;21:1390-1395. [DOI:10.1007/s00167-012-2252-7] [PMID]
6. Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow‐up after ankle inversion trauma. Scandinavian journal of medicine & science in sports. 2002;12(3):129-135. [DOI:10.1034/j.1600-0838.2002.02104.x] [PMID]
7. Hertel J, Corbett RO. An updated model of chronic ankle instability. Journal of athletic training. 2019;54(6):572-588. [DOI:10.4085/1062-6050-344-18] [PMID]
8. McCann RS, Crossett ID, Terada M, Kosik KB, Bolding BA, Gribble PA. Hip strength and star excursion balance test deficits of patients with chronic ankle instability. Journal of science and medicine in sport. 2017;20(11):992-996. [DOI:10.1016/j.jsams.2017.05.005] [PMID]
9. Mohammadpour N, Rezaie I, Hadadi M. The Relationship between Core Muscles Dysfunction and Chronic Ankle Instability: A Review. Journal of Sport Biomechanics. 2019;5(2):72-81. [DOI:10.32598/biomechanics.5.2.4]
10. Delahunt E, Monaghan K, Caulfield B. Ankle function during hopping in subjects with functional instability of the ankle joint. Scandinavian journal of medicine & science in sports. 2007;17(6):641-648. [DOI:10.1111/j.1600-0838.2006.00612.x] [PMID]
11. Wikstrom E, Tillman M, Chmielewski T, Cauraugh J, Naugle K, Borsa P. Dynamic postural control but not mechanical stability differs among those with and without chronic ankle instability. Scandinavian journal of medicine & science in sports. 2010;20(1):e137-e144. [DOI:10.1111/j.1600-0838.2009.00929.x] [PMID]
12. Riemann BL. Is there a link between chronic ankle instability and postural instability? Journal of athletic training. 2002;37(4):386.
13. Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. Journal of athletic training. 2012;47(3):339-357. [DOI:10.4085/1062-6050-47.3.08] [PMID]
14. McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part I: can deficits be detected with instrumented testing? Journal of athletic training. 2008;43(3):293-304. [DOI:10.4085/1062-6050-43.3.293] [PMID]
15. Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Borsa PA. Dynamic postural stability deficits in subjects with self-reported ankle instability. Medicine & Science in Sports & Exercise. 2007;39(3):397-402. [DOI:10.1249/mss.0b013e31802d3460] [PMID]
16. Hadadi M, Abbasi F. Comparison of the effect of the combined mechanism ankle support on static and dynamic postural control of chronic ankle instability patients. Foot & ankle international. 2019;40(6):702-709. [DOI:10.1177/1071100719833993] [PMID]
17. Hopkins JT, Coglianese M, Glasgow P, Reese S, Seeley MK. Alterations in evertor/invertor muscle activation and center of pressure trajectory in participants with functional ankle instability. Journal of Electromyography and Kinesiology. 2012;22(2):280-285. [DOI:10.1016/j.jelekin.2011.11.012] [PMID]
18. Jaber H, Lohman E, Daher N, Bains G, Nagaraj A, Mayekar P, et al. Neuromuscular control of ankle and hip during performance of the star excursion balance test in subjects with and without chronic ankle instability. PloS one. 2018;13(8):e0201479. [DOI:10.1371/journal.pone.0201479] [PMID]
19. Yousefi M, Sadeghi H, Ilbiegi S, Ebrahimabadi Z, Kakavand M, Wikstrom EA. Center of pressure excursion and muscle activation during gait initiation in individuals with and without chronic ankle instability. Journal of Biomechanics. 2020;108:109904. [DOI:10.1016/j.jbiomech.2020.109904] [PMID]
20. Oh M, Lee H, Han S, Hopkins JT. Postural control measured before and after simulated ankle inversion landings among individuals with chronic ankle instability, copers, and controls. Gait & Posture. 2024;107:17-22. [DOI:10.1016/j.gaitpost.2023.09.002] [PMID]
21. Liu Y, Song Q, Zhou Z, Chen Y, Wang J, Tian X, et al. Effects of fatigue on balance and ankle proprioception during drop landing among individuals with and without chronic ankle instability. Journal of Biomechanics. 2023;146:111431. [DOI:10.1016/j.jbiomech.2022.111431] [PMID]
22. Kawaguchi K, Taketomi S, Mizutani Y, Inui H, Yamagami R, Kono K, et al. Dynamic postural stability is decreased during the single-leg drop landing task in male collegiate soccer players with chronic ankle instability. Orthopaedic Journal of Sports Medicine. 2022;10(7):23259671221107343. [DOI:10.1177/23259671221107343] [PMID]
23. Simpson JD, Koldenhoven RM, Wilson SJ, Stewart EM, Turner AJ, Chander H, et al. Ankle kinematics, center of pressure progression, and lower extremity muscle activity during a side-cutting task in participants with and without chronic ankle instability. Journal of Electromyography and Kinesiology. 2020;54:102454. [DOI:10.1016/j.jelekin.2020.102454] [PMID]
24. Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT-P, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. British journal of sports medicine. 2016;50(24):1496-1505. [DOI:10.1136/bjsports-2016-096189]
25. Dundas MA, Gutierrez GM, Pozzi F. Neuromuscular control during stepping down in continuous gait in individuals with and without ankle instability. Journal of sports sciences. 2014;32(10):926-933. [DOI:10.1080/02640414.2013.868917] [PMID]
26. Watabe T, Takabayashi T, Tokunaga Y, Kubo M. Copers adopt an altered dynamic postural control compared to individuals with chronic ankle instability and controls in unanticipated single-leg landing. Gait & Posture. 2022;92:378-382. [DOI:10.1016/j.gaitpost.2021.12.014] [PMID]
27. Ma T, Li Q, Song Y, Hua Y. Chronic ankle instability is associated with proprioception deficits: a systematic review and meta-analysis. Journal of sport and health science. 2021;10(2):182-191. [DOI:10.1016/j.jshs.2020.09.014] [PMID]
28. Farhadi MHI, Seidi F, Minoonejad H, Thomas AC. Differences in gluteal and quadriceps muscle activation among adults with and without lumbar hyperlordosis. Journal of sport rehabilitation. 2020;29(8):1100-1105. [DOI:10.1123/jsr.2019-0112] [PMID]
29. Kim H-J, Lee J-H, Lee D-H. Proprioception in patients with anterior cruciate ligament tears: a meta-analysis comparing injured and uninjured limbs. The American journal of sports medicine. 2017;45(12):2916-2922. [DOI:10.1177/0363546516682231] [PMID]
30. Needle AR, Lepley AS, Grooms DR. Central nervous system adaptation after ligamentous injury: a summary of theories, evidence, and clinical interpretation. Sports medicine. 2017;47:1271-1288. [DOI:10.1007/s40279-016-0666-y] [PMID]
31. Kapreli E, Athanasopoulos S. The anterior cruciate ligament deficiency as a model of brain plasticity. Medical hypotheses. 2006;67(3):645-650. [DOI:10.1016/j.mehy.2006.01.063] [PMID]
32. Simpson JD, Stewart EM, Macias DM, Chander H, Knight AC. Individuals with chronic ankle instability exhibit dynamic postural stability deficits and altered unilateral landing biomechanics: A systematic review. Physical Therapy in Sport. 2019;37:210-219. [DOI:10.1016/j.ptsp.2018.06.003] [PMID]
33. Labanca L, Mosca M, Ghislieri M, Agostini V, Knaflitz M, Benedetti MG. Muscle activations during functional tasks in individuals with chronic ankle instability: a systematic review of electromyographical studies. Gait & posture. 2021;90:340-373. [DOI:10.1016/j.gaitpost.2021.09.182] [PMID]
34. Pintsaar A, Brynhildsen J, Tropp H. Postural corrections after standardised perturbations of single limb stance: effect of training and orthotic devices in patients with ankle instability. British journal of sports medicine. 1996;30(2):151-155. [DOI:10.1136/bjsm.30.2.151] [PMID]
35. Tropp H. Commentary: functional ankle instability revisited. Journal of athletic training. 2002;37(4):512.
36. Azadian E, Eftekhari N, Mohammad Zaheri R. The Evaluation of Changes in the Center of Pressure in Different Types of Defense on the Professional Volleyball Players. Journal of Sport Biomechanics. 2022;8(3):266-278. [DOI:10.61186/JSportBiomech.8.3.266]
37. Simpson JD, Stewart EM, Turner AJ, Macias DM, Wilson SJ, Chander H, et al. Neuromuscular control in individuals with chronic ankle instability: a comparison of unexpected and expected ankle inversion perturbations during a single leg drop-landing. Human Movement Science. 2019;64:133-141. [DOI:10.1016/j.humov.2019.01.013] [PMID]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |