Volume 11, Issue 3 (12-2025)
J Sport Biomech 2025, 11(3): 288-304 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Salimi K, Nakhaei K, Tabatabai Ghomsheh S F, Tehrani P, Shojaei S. Comparison of Kinetic and Kinematic Parameters of Walking Between Healthy Individuals and Patients with Heart Disease. J Sport Biomech 2025; 11 (3) :288-304
URL: http://biomechanics.iauh.ac.ir/article-1-375-en.html
URL: http://biomechanics.iauh.ac.ir/article-1-375-en.html
Kamran Salimi1 

 , Koorosh Nakhaei *2
, Koorosh Nakhaei *2 

 , Seyed Farhad Tabatabai Ghomsheh3
, Seyed Farhad Tabatabai Ghomsheh3 

 , Pedram Tehrani1
, Pedram Tehrani1 

 , Shahrokh Shojaei1
, Shahrokh Shojaei1 




 , Koorosh Nakhaei *2
, Koorosh Nakhaei *2 

 , Seyed Farhad Tabatabai Ghomsheh3
, Seyed Farhad Tabatabai Ghomsheh3 

 , Pedram Tehrani1
, Pedram Tehrani1 

 , Shahrokh Shojaei1
, Shahrokh Shojaei1 


1- Department of Biomedical Engineering, CT.C., Islamic Azad University, Tehran, Iran.
2- Department of Biomedical Engineering, Faculty of Technology and Engineering, Islamshahr Branch, Islamic Azad University, Islamshahr, Iran.
3- Pediatric Neurorehabilitation Research Center, Ergonomics Department, Faculty of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Biomedical Engineering, Faculty of Technology and Engineering, Islamshahr Branch, Islamic Azad University, Islamshahr, Iran.
3- Pediatric Neurorehabilitation Research Center, Ergonomics Department, Faculty of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Full-Text [PDF 2108 kb]
(403 Downloads)
| Abstract (HTML) (1473 Views)
Full-Text: (443 Views)
Extended Abstract
1. Introduction
Cardiovascular diseases (CVD), particularly chronic heart failure (CHF), represent a major global public health challenge and remain among the leading causes of mortality and morbidity worldwide. CHF affects over 26 million individuals globally, with its prevalence steadily rising due to aging populations and lifestyle-related risk factors such as hypertension, obesity, diabetes, and physical inactivity. CVD encompasses a broad spectrum of conditions, including coronary artery disease, myocardial infarction, arrhythmias, and peripheral artery disease. Among these, CHF is especially debilitating due to its progressive nature, which leads to fatigue, dyspnea, reduced physical capacity, and a markedly diminished quality of life. One of the less-explored consequences of CHF is its impact on neuromuscular coordination and locomotor function, particularly gait performance. Evidence suggests that individuals with CHF often exhibit abnormal gait patterns due to muscle weakness, balance impairments, early onset of fatigue, and compensatory movement strategies—all of which contribute to an increased risk of falls and further physical decline. Despite the clinical relevance of gait biomechanics in understanding functional limitations in CHF, the routine use of gait analysis in clinical practice remains limited. A comprehensive biomechanical assessment of gait has the potential to detect early signs of functional deterioration and inform personalized rehabilitation strategies. Therefore, the present study aims to examine the differences in gait kinematics and kinetics between patients with CHF and healthy controls, focusing on joint angles and joint moments across multiple planes of motion. These insights may enhance our understanding of functional deficits in CHF and support the development of targeted therapeutic interventions.
2. Methods
This case-control study included a total of 40 participants: 20 patients diagnosed with CVD, specifically chronic heart failure (CHF), and 20 age- and BMI-matched healthy controls. The patients (mean age = 53.7 ± 9.5 years; mean BMI = 22.5 ± 4.5) were referred by cardiologists and had confirmed CHF diagnoses based on clinical evaluation and echocardiographic findings. Exclusion criteria were the presence of musculoskeletal disorders, neurological impairments, or any other conditions that could affect gait performance. Gait data were collected using a high-resolution three-dimensional motion capture system (Basler, Germany) operating at 200 Hz with a 7K resolution. Reflective markers were bilaterally placed on key anatomical landmarks following a standardized biomechanical model (e.g., Plug-in Gait). Simultaneously, ground reaction forces were recorded using a Kistler force plate (Kistler, Switzerland) at a sampling frequency of 1000 Hz. Participants performed multiple walking trials on a 10-meter walkway at their self-selected comfortable speed. The most consistent and representative gait cycles were selected for analysis. Kinematic parameters included joint angles and ranges of motion, while kinetic parameters focused on joint torques and ground reaction forces, specifically in the sagittal, frontal, and transverse planes. To maintain consistency, only data from the dominant limb were analyzed. All data were processed and filtered using standard biomechanical protocols. Statistical analyses were performed using SPSS version 23. Independent t-tests were used for normally distributed variables, and Mann–Whitney U tests were applied for non-normally distributed variables. A significance level of p < 0.05 was considered statistically significant.
3. Results
The findings revealed significant alterations in joint torque patterns among patients with CHF compared to healthy controls. In the sagittal plane, reduced ankle plantarflexion torque during push-off (p = 0.045), decreased knee extension torque (p = 0.010), and diminished hip extension torque at heel contact (p = 0.030) were observed. Frontal plane analysis showed a significant reduction in knee varus torque during early stance (p = 0.021) and hip adduction torque during mid-stance (p = 0.027). In the transverse plane, both knee external rotation torque (p = 0.038) and hip internal rotation torque (p = 0.042) were significantly lower in CHF patients (Fig. 1). Joint range of motion (ROM) was also significantly reduced, particularly in knee flexion during the swing phase (p = 0.002) and in total hip motion (p = 0.005).
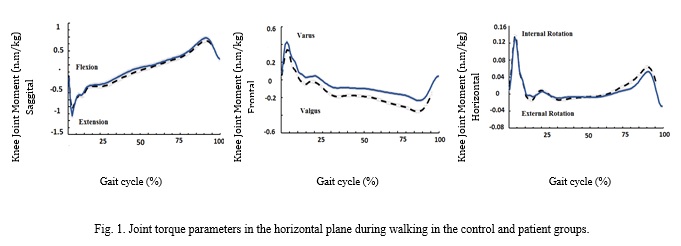
Significant differences in ground reaction forces (GRF) were found only in the sagittal plane, where both mean (p = 0.009) and minimum values (p = 0.011) were higher in patients compared to controls. However, joint stiffness did not show statistically significant differences across all planes, likely due to considerable inter-subject variability and overlapping values. Kinematic analysis indicated relatively higher mean hip angles in the sagittal plane among CHF patients, possibly reflecting a compensatory strategy to maintain propulsion and balance. The observed reductions in hip and knee extensor torques suggest underlying neuromuscular weakness or impaired motor control mechanisms. Overall, gait in CHF patients appeared less efficient and more variable, underscoring the need for comprehensive biomechanical assessment and individualized rehabilitation strategies aimed at addressing functional deficits and enhancing postural stability.
4. Discussion
This study demonstrated that chronic heart failure (CHF) significantly affects gait biomechanics. Compared to healthy controls, patients with CHF exhibited marked alterations in joint kinematics, kinetics, joint stiffness, and ground reaction forces (GRFs) across the sagittal, frontal, and transverse planes. In the sagittal plane, significant reductions in ankle plantarflexion and dorsiflexion moments during push-off, along with decreased hip and knee range of motion during the swing phase, indicated impaired propulsion and diminished lower limb functionality. Although differences in joint angles and stiffness in the frontal plane did not reach statistical significance, CHF patients exhibited reduced adduction/abduction moments and limited lateral knee motion. These findings suggest weakness in stabilizing musculature and compromised balance control. In the transverse plane, decreased rotational moments and reduced range of motion at the hip and knee, combined with increased ankle rotational moments, pointed to compensatory strategies aimed at mitigating unwanted rotational instability. Joint stiffness did not differ significantly between groups in any plane. The high inter-subject variability and overlapping standard deviations limited its clinical utility as a discriminative measure. GRF analysis revealed statistically significant differences only in the sagittal plane, particularly in variability and peak loading, underscoring the relevance of this parameter in clinical gait assessment. Notably, CHF patients exhibited increased hip joint angles, elevated ankle rotational moments, and reduced sagittal plane moments at proximal joints. These patterns reflect diminished gait efficiency and heightened postural instability. The findings underscore the importance of a multidimensional gait assessment approach—integrating biomechanical and neuromechanical metrics—and support the development of tailored rehabilitation programs to enhance functional mobility and balance in individuals with CHF.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be addressed in this research.
Funding
This research did not receive any financial support from government, private, or non-profit organizations.
Authors' contributions
All authors contributed equally to preparing the article.
Conflicts of interest
The authors declare that there are no conflicts of interest associated with this article.
1. Introduction
Cardiovascular diseases (CVD), particularly chronic heart failure (CHF), represent a major global public health challenge and remain among the leading causes of mortality and morbidity worldwide. CHF affects over 26 million individuals globally, with its prevalence steadily rising due to aging populations and lifestyle-related risk factors such as hypertension, obesity, diabetes, and physical inactivity. CVD encompasses a broad spectrum of conditions, including coronary artery disease, myocardial infarction, arrhythmias, and peripheral artery disease. Among these, CHF is especially debilitating due to its progressive nature, which leads to fatigue, dyspnea, reduced physical capacity, and a markedly diminished quality of life. One of the less-explored consequences of CHF is its impact on neuromuscular coordination and locomotor function, particularly gait performance. Evidence suggests that individuals with CHF often exhibit abnormal gait patterns due to muscle weakness, balance impairments, early onset of fatigue, and compensatory movement strategies—all of which contribute to an increased risk of falls and further physical decline. Despite the clinical relevance of gait biomechanics in understanding functional limitations in CHF, the routine use of gait analysis in clinical practice remains limited. A comprehensive biomechanical assessment of gait has the potential to detect early signs of functional deterioration and inform personalized rehabilitation strategies. Therefore, the present study aims to examine the differences in gait kinematics and kinetics between patients with CHF and healthy controls, focusing on joint angles and joint moments across multiple planes of motion. These insights may enhance our understanding of functional deficits in CHF and support the development of targeted therapeutic interventions.
2. Methods
This case-control study included a total of 40 participants: 20 patients diagnosed with CVD, specifically chronic heart failure (CHF), and 20 age- and BMI-matched healthy controls. The patients (mean age = 53.7 ± 9.5 years; mean BMI = 22.5 ± 4.5) were referred by cardiologists and had confirmed CHF diagnoses based on clinical evaluation and echocardiographic findings. Exclusion criteria were the presence of musculoskeletal disorders, neurological impairments, or any other conditions that could affect gait performance. Gait data were collected using a high-resolution three-dimensional motion capture system (Basler, Germany) operating at 200 Hz with a 7K resolution. Reflective markers were bilaterally placed on key anatomical landmarks following a standardized biomechanical model (e.g., Plug-in Gait). Simultaneously, ground reaction forces were recorded using a Kistler force plate (Kistler, Switzerland) at a sampling frequency of 1000 Hz. Participants performed multiple walking trials on a 10-meter walkway at their self-selected comfortable speed. The most consistent and representative gait cycles were selected for analysis. Kinematic parameters included joint angles and ranges of motion, while kinetic parameters focused on joint torques and ground reaction forces, specifically in the sagittal, frontal, and transverse planes. To maintain consistency, only data from the dominant limb were analyzed. All data were processed and filtered using standard biomechanical protocols. Statistical analyses were performed using SPSS version 23. Independent t-tests were used for normally distributed variables, and Mann–Whitney U tests were applied for non-normally distributed variables. A significance level of p < 0.05 was considered statistically significant.
3. Results
The findings revealed significant alterations in joint torque patterns among patients with CHF compared to healthy controls. In the sagittal plane, reduced ankle plantarflexion torque during push-off (p = 0.045), decreased knee extension torque (p = 0.010), and diminished hip extension torque at heel contact (p = 0.030) were observed. Frontal plane analysis showed a significant reduction in knee varus torque during early stance (p = 0.021) and hip adduction torque during mid-stance (p = 0.027). In the transverse plane, both knee external rotation torque (p = 0.038) and hip internal rotation torque (p = 0.042) were significantly lower in CHF patients (Fig. 1). Joint range of motion (ROM) was also significantly reduced, particularly in knee flexion during the swing phase (p = 0.002) and in total hip motion (p = 0.005).
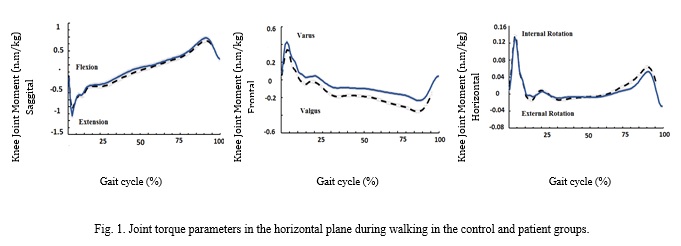
Significant differences in ground reaction forces (GRF) were found only in the sagittal plane, where both mean (p = 0.009) and minimum values (p = 0.011) were higher in patients compared to controls. However, joint stiffness did not show statistically significant differences across all planes, likely due to considerable inter-subject variability and overlapping values. Kinematic analysis indicated relatively higher mean hip angles in the sagittal plane among CHF patients, possibly reflecting a compensatory strategy to maintain propulsion and balance. The observed reductions in hip and knee extensor torques suggest underlying neuromuscular weakness or impaired motor control mechanisms. Overall, gait in CHF patients appeared less efficient and more variable, underscoring the need for comprehensive biomechanical assessment and individualized rehabilitation strategies aimed at addressing functional deficits and enhancing postural stability.
4. Discussion
This study demonstrated that chronic heart failure (CHF) significantly affects gait biomechanics. Compared to healthy controls, patients with CHF exhibited marked alterations in joint kinematics, kinetics, joint stiffness, and ground reaction forces (GRFs) across the sagittal, frontal, and transverse planes. In the sagittal plane, significant reductions in ankle plantarflexion and dorsiflexion moments during push-off, along with decreased hip and knee range of motion during the swing phase, indicated impaired propulsion and diminished lower limb functionality. Although differences in joint angles and stiffness in the frontal plane did not reach statistical significance, CHF patients exhibited reduced adduction/abduction moments and limited lateral knee motion. These findings suggest weakness in stabilizing musculature and compromised balance control. In the transverse plane, decreased rotational moments and reduced range of motion at the hip and knee, combined with increased ankle rotational moments, pointed to compensatory strategies aimed at mitigating unwanted rotational instability. Joint stiffness did not differ significantly between groups in any plane. The high inter-subject variability and overlapping standard deviations limited its clinical utility as a discriminative measure. GRF analysis revealed statistically significant differences only in the sagittal plane, particularly in variability and peak loading, underscoring the relevance of this parameter in clinical gait assessment. Notably, CHF patients exhibited increased hip joint angles, elevated ankle rotational moments, and reduced sagittal plane moments at proximal joints. These patterns reflect diminished gait efficiency and heightened postural instability. The findings underscore the importance of a multidimensional gait assessment approach—integrating biomechanical and neuromechanical metrics—and support the development of tailored rehabilitation programs to enhance functional mobility and balance in individuals with CHF.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be addressed in this research.
Funding
This research did not receive any financial support from government, private, or non-profit organizations.
Authors' contributions
All authors contributed equally to preparing the article.
Conflicts of interest
The authors declare that there are no conflicts of interest associated with this article.
Type of Study: Applicable |
Subject:
Special
Received: 2025/04/19 | Accepted: 2025/07/29 | Published: 2025/07/29
Received: 2025/04/19 | Accepted: 2025/07/29 | Published: 2025/07/29
References
1. Chahal J, Gómez-Aristizábal A, Shestopaloff K, Bhatt S, Chaboureau A, Fazio A, et al. Bone marrow mesenchymal stromal cell treatment in patients with osteoarthritis results in overall improvement in pain and symptoms and reduces synovial inflammation. Stem cells translational medicine. 2019;8(8):746-57. [DOI:10.1002/sctm.18-0183] [PMID]
2. Enayati M, Mardani-Hamooleh M, Farahani Nia M, Haghani S. Relationship between spiritual intelligence and illness-related worries in hospitalized patients with heart failure in Mazandaran, Iran. Iran Journal of Nursing. 2022;35(138):434-47. [DOI:10.32598/ijn.35.138.764.29]
3. Maghsodi H, Ebrahimi M, Ghanbari A, Hejaziyan SH. Investigation of the Anti-inflammatory Properties of Iranian Nigella sativa L in Reducing the Expression of Pre-Inflammatory Cytokines of TNF-α and IL-18 in Human THP-1 Cells. Journal of Ilam University of Medical Sciences. 2017;25(3):147-59. [DOI:10.29252/sjimu.25.3.147]
4. Arnold EM, Ward SR, Lieber RL, Delp SL. A model of the lower limb for analysis of human movement. Annals of biomedical engineering. 2010;38:269-79. [DOI:10.1007/s10439-009-9852-5] [PMID]
5. Panizzolo FA, Maiorana AJ, Naylor LH, Lichtwark GA, Dembo L, Lloyd DG, et al. Is the soleus a sentinel muscle for impaired aerobic capacity in heart failure? Medicine and science in sports and exercise. 2015;47(3):498-508. [DOI:10.1249/MSS.0000000000000431] [PMID]
6. Rezaei M, Najafian Razavi M, Mazandarani E. The Kinematics Gait Pattern Analysis of Thin, Normal and Obese Children. Journal of Sport Biomechanics. 2018;4(2):49-57.
7. Forman DE, Fleg JL, Kitzman DW, Brawner CA, Swank AM, McKelvie RS, et al. 6-min walk test provides prognostic utility comparable to cardiopulmonary exercise testing in ambulatory outpatients with systolic heart failure. Journal of the American College of Cardiology. 2012;60(25):2653-61. [DOI:10.1016/j.jacc.2012.08.1010] [PMID]
8. Najafian Razavi M. The Comparison of Gait Kinematics in Over-Weight and Normal-Weight People across Age Groups. Journal of Sport Biomechanics. 2022;8(3):214-30. [DOI:10.61186/JSportBiomech.8.3.214]
9. Hasandokht T, Salari A, Salari A, Fazeli A, Ashkan M. Evaluation of relation between cardiovascular risk factors and osteoarthritis: Results of a cross-sectional Study. Feyz Medical Sciences Journal. 2019;23(2):209-15.
10. McGibbon CA, Krebs DE, Puniello MS. Mechanical energy analysis identifies compensatory strategies in disabled elders' gait. Journal of biomechanics. 2001;34(4):481-90. [DOI:10.1016/S0021-9290(00)00220-7] [PMID]
11. Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest. 1996;110(2):325-32. [DOI:10.1378/chest.110.2.325] [PMID]
12. Shokrallahnia-Roshan A, Sadeghi H, Shirani S, Nejatian M. Effects of Strength Training and Cardiac Rehabilitation Programs on the Biomechanical Parameters of Blood Flow Velocity and Blood Flow Rate and Its Relation With Arterial Stiffness Index in Brachial and Femoral Arteries with Coronary Artery Bypass Grafting Patients (CABG). Archives of Rehabilitation. 2013;14(2):38-45.
13. Gibbs N, Diamond R, Sekyere EO, Thomas WD. Management of knee osteoarthritis by combined stromal vascular fraction cell therapy, platelet-rich plasma, and musculoskeletal exercises: a case series. Journal of pain research. 2015:799-806. [DOI:10.2147/JPR.S92090] [PMID]
14. Masoli M, Fabian D, Holt S, Beasley R, Program GIfA. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004;59(5):469-78. [DOI:10.1111/j.1398-9995.2004.00526.x] [PMID]
15. Razaghi A, Sadeghi H, Johari Moghadam A, azma k, Motamedi P. The Effect of Exercise-Based Cardiac Rehabilitation In two ways Aerobic and Aerobic-Resistance Exercises on the Biomechanical Function of Cardiac Patients (MI, PCI, and CABG). Razi Journal of Medical Sciences. 2020;26(12):138-48.
16. Boyd R, Fatone S, Rodda J, Olesch C, Starr R, Cullis E, et al. High-or low-technology measurements of energy expenditure in clinical gait analysis? Developmental Medicine and Child Neurology. 1999;41(10):676-82. [DOI:10.1111/j.1469-8749.1999.tb00522.x] [PMID]
17. Celis R, Pipinos II, Scott-Pandorf MM, Myers SA, Stergiou N, Johanning JM. Peripheral arterial disease affects kinematics during walking. Journal of vascular surgery. 2009;49(1):127-32. [DOI:10.1016/j.jvs.2008.08.013] [PMID]
18. The Criteria Committee of the New York Heart Association. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th ed. Boston, MA: Little, Brown & Co; 1994. p. 253-256.
19. Karatsidis A, Jung M, Schepers HM, Bellusci G, de Zee M, Veltink PH, et al. Predicting kinetics using musculoskeletal modeling and inertial motion capture. arXiv preprint 2018. arXiv:180101668.
20. Panizzolo FA, Maiorana A, Naylor LH, Rubenson J. Gait analysis in chronic heart failure: The calf as a locus of impaired walking capacity. Journal of Biomechanics. 2014;47(15):3719-25. [DOI:10.1016/j.jbiomech.2014.09.015] [PMID]
21. Ozcan EB, Saglam M, Vardar-Yagli N, et al. Impaired balance and gait characteristics in patients with chronic heart failure. Heart Lung Circulation. 2022;31(6):832-40. [DOI:10.1016/j.hlc.2021.10.015] [PMID]
22. Crespo-Ruiz B, Del Rosario-Garrido M, Cuesta-Vargas AI. Kinematic analysis of gait in patients with heart failure and controls: A cross-sectional study. Gait Posture. 2017;55:36-41.
23. Neptune RR, Zajac FE, Kautz SA. Muscle force redistributions during walking in persons with post-stroke hemiparesis. Journal of Biomechanics. 2004;37(6):403-12. [DOI:10.1016/j.jbiomech.2003.11.001] [PMID]
24. Heiden TL, Sandroff BM, Motl RW. Biomechanical and energetic determinants of walking performance in multiple sclerosis. Clinical Biomechanics. 2016;33:6-11.
25. Eng JJ, Winter DA. Kinetic analysis of human walking: Data interpretation and recommendations for improvement. Physical Therapy. 1995;75(9):776-85.
26. Ogaya S. Joint stiffness in patients with heart failure: a pilot study using gait analysis. Clinical Biomechanics. 2020;74:20-6.
27. Ozcan EB, Saglam M, Vardar-Yagli N, et al. Impaired balance and gait characteristics in patients with chronic heart failure. Heart, Lung and Circulation. 2022;31(6):832-40. [DOI:10.1016/j.hlc.2021.10.015] [PMID]
28. Neptune RR, Kautz SA, Zajac FE. Contributions of the individual ankle plantar flexors to support, forward progression and swing initiation during walking. Journal of Biomechanics. 2001;34(11):1387-98. [DOI:10.1016/S0021-9290(01)00105-1] [PMID]
29. Crespo-Ruiz B, Cuesta-Vargas AI. Kinematic analysis of gait in patients with heart failure and controls: A cross-sectional study. Gait & Posture. 2017;55:36-41.
30. Barker K, et al. Ground reaction force characteristics in patients with chronic heart failure. European Journal of Physical and Rehabilitation Medicine. 2013;49(3):351-7.
31. Dingwell JB, Cusumano JP. Nonlinear time series analysis of normal and pathological human walking. Chaos. 2000;10(4):848-63. [DOI:10.1063/1.1324008] [PMID]
32. Rahman H, Pipinos II, Johanning JM, Myers SA. Gait variability is affected more by peripheral artery disease than by vascular occlusion. Public Library of Science. 2021;16(3):e0241727. [DOI:10.1371/journal.pone.0241727] [PMID]
33. Piri A, Jafarnejadgero A, Ebrahimipour H, Nasri S. A review of the effects of exercise on body mechanics during translational movements in individuals with foot pronation: 2019-2022. Journal of Shahid Sadoughi University of Medical Sciences. 2023; 31(4):6544-60. [DOI:10.18502/ssu.v31i4.13024]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |