Volume 11, Issue 3 (12-2025)
J Sport Biomech 2025, 11(3): 306-325 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Diniz R F, Chivate D, Motimath B. Prevalence of Sacroiliac Joint Dysfunction Among Young Badminton Players. J Sport Biomech 2025; 11 (3) :306-325
URL: http://biomechanics.iauh.ac.ir/article-1-401-en.html
URL: http://biomechanics.iauh.ac.ir/article-1-401-en.html
1- Department of Sports Physiotherapy, KLE Institute of Physiotherapy, Belagavi, Karnataka, India.
Full-Text [PDF 2018 kb]
(411 Downloads)
| Abstract (HTML) (1740 Views)
Full-Text: (657 Views)
1. Introduction
Badminton is one of the most popular sports globally, with nearly 200 million individuals playing at various proficiency levels (1, 2). Known as the "fastest racket sport" due to its high tempo (2), badminton places unique demands on athletes. The game's rapid pace requires players to anticipate and react within fractions of a second, creating a dynamic and exhilarating environment (2, 3). As a physically demanding sport, badminton involves a wide range of movements that require speed, strength, agility, and explosive action. Players perform complex footwork patterns including lunging, pivoting, leaping, overhead smashes, sudden directional changes, and rapid acceleration and deceleration. These movements demand quick postural adjustments to maintain balance and prepare for subsequent shots (3). Such requirements impose substantial strain on the musculoskeletal system, particularly the trunk, lower extremities, and core muscles, which are constantly engaged during both offensive and defensive play (4). These biomechanical demands increase the risk of musculoskeletal injuries, especially among younger athletes (2).
Previous studies have reported that badminton players face an injury rate of approximately 0.85 injuries per year, 1.6–2.9 injuries per 1,000 hours of play, 2–5 injuries per 1,000 players, and account for 1%–5% of all sports-related injuries (5, 6). Of these, 58%–76% involve the lower limbs, 11%–16% the upper limbs, and 11%–16% the back (3, 7). The prevalence of low back pain (LBP) among badminton players has been estimated at 12.9% (4). Bhagat et al. (2022) (2) identified a significant prevalence of lower back and lower extremity injuries among badminton players in Vadodara, often linked to overuse, poor biomechanics, and inadequate fitness—factors also associated with sacroiliac joint dysfunction (SIJD). Similarly, Ejaz et al. (2023) (4) reported frequent musculoskeletal complaints, particularly in the lumbar spine, shoulders, and lower limbs, among players in Pakistan’s twin cities. These findings highlight the vulnerability of the lower back and pelvic regions in badminton athletes and suggest a potential underlying role of SIJ dysfunction. Despite these findings, research specifically addressing SIJD in badminton remains limited. In their comprehensive review of badminton-related injuries, Phomsoupha et al. (2020) (3) noted that although LBP is commonly reported, the SIJ is rarely identified as the specific source of pain. The SIJ is often overlooked in clinical evaluations due to diagnostic challenges and the overlap of symptoms with hip and lumbar spine disorders. However, considering badminton’s unique biomechanical demands—such as abrupt lunges, trunk rotations, and asymmetrical loading during rallies—the SIJ is likely subjected to significant mechanical stress (8, 9).
The importance of SIJD in the athletic context is further supported by Abdollahi et al. (2023) (9), who reported a strong correlation between SIJD and previous lower limb sports injuries. Their findings suggest that altered gait and loading patterns may increase SIJ stress (9, 10). This supports the concept of kinetic chain dysfunction and underscores the importance of evaluating SIJ integrity in athletes with recurrent leg, pelvic, or low back pain—particularly in young badminton players, who may adopt compensatory movement patterns due to ongoing musculoskeletal development. Sacroiliac joint dysfunction can significantly affect lower limb biomechanics, leading to pelvic asymmetry, restricted hip and knee mobility, and abnormal gait patterns, thereby increasing long-term injury risk (11). Early detection and intervention are crucial to preventing chronic pain and functional decline. The high-intensity demands of badminton can place substantial stress on the SIJ, making players more susceptible to dysfunction. Despite the joint's vital role in pelvic stability and load transmission, limited data exist regarding SIJD prevalence in badminton players (9).
This study aims to fill that gap. Determining the prevalence of SIJD among young badminton players can help identify sport-specific injury patterns. With such insights, targeted preventive strategies can be developed. Furthermore, early diagnosis of SIJD—given its impact on discomfort, mobility, and stability—can help optimize player performance. Ultimately, raising awareness among athletes, coaches, and healthcare professionals promotes a proactive approach to injury management and enriches the broader field of sports medicine.
2. Methods
2.1. Subjects
A cross-sectional study was carried out among badminton players in Belagavi city from November 2024 to May 2025, resulting in a final sample size of 77 participants. The required sample size was calculated using the standard formula:
n = [2(Zₐ + Zᵦ)² × p × q] / d²,
where n represents the sample size, Zₐ is the standard normal deviate corresponding to the desired confidence level (1.96 for 5%), Zᵦ denotes the standard normal deviate associated with the desired power (0.84 for 80%), p is the estimated prevalence (45%), q is 1 minus p (i.e., 55%), and d is the clinically meaningful effect size, set at 22.5%. By substituting these values into the formula, the calculated sample size was 77.
The estimated prevalence of 45% was selected based on previous literature addressing musculoskeletal dysfunctions such as low back pain and sacroiliac joint dysfunction (SIJD) in adolescent athletes. Although specific prevalence data for SIJD among badminton players is limited, studies involving similar athletic populations—such as runners, football players, and adolescent athletes in general—report prevalence rates ranging from 30% to 50%. Therefore, a midpoint estimate of 45% was deemed both conservative and realistic. The effect size of 22.5% was chosen based on two key considerations: first, the exploratory nature of this study as one of the earliest investigations into SIJD prevalence in adolescent badminton players, justifying a broader margin of error; and second, feasibility constraints, since detecting smaller effect sizes (e.g., 10–15%) would have required a substantially larger sample size, which was not practical due to the limited number of registered players in the region. Although 22.5% slightly exceeds the typical range of 10–20%, it was considered acceptable for an initial prevalence study with moderate statistical power.
Eligible participants were male and female badminton players aged between 14 and 22 years, each with at least 1.5 to 2 years of playing experience and a minimum of three training sessions per week on synthetic surfaces. Players with a body mass index (BMI) greater than 15 kg/m² were included, and only those who provided signed informed consent (or assent in the case of minors) were enrolled in the study. Exclusion criteria included active low back or buttock pain (e.g., due to prolapsed intervertebral disc or sciatica), recent fractures, lower limb injuries or surgeries within the past six months, and any diagnosed neurological or cardiovascular conditions.
2.2. Procedure
Prior to the commencement of the study, ethical clearance was obtained from the Institutional Ethics Review Committee. The study was also registered with the Clinical Trials Registry – India (CTRI), under the registration number CTRI/2024/12/077547. The study began by identifying the total number of badminton academies in Belagavi, from which two academies were selected randomly. Participants were screened based on the inclusion and exclusion criteria, and simple random sampling was used to select individuals from the list of registered players at each academy. The purpose of the study was clearly explained to each selected participant, and informed consent or assent was obtained prior to participation.
2.3. Outcome Measures
SIJD was evaluated using five standardized special tests administered in random order. A diagnosis of dysfunction was considered positive if three or more tests yielded positive results. Previous studies have shown that having three or more positive maneuvers provides a sensitivity of 94% and a specificity of 78% for diagnosing SIJ dysfunction. The tests used were Patrick’s FABER test, compression test, thigh thrust test, distraction test, and Gaenslen’s test (9, 10, 12). A test was deemed positive if it reproduced the subject’s familiar pain or discomfort in the SIJ region during the maneuver.
Descriptions of the SIJ Clinical Tests:
• Patrick’s FABER Test: The patient lies in a supine position while the examiner stands beside them. The examiner brings the ipsilateral hip into flexion, abduction, and external rotation, with the knee flexed so the heel rests on the contralateral knee. The examiner stabilizes the contralateral anterior superior iliac spine (ASIS) and applies posteriorly directed pressure to the flexed knee. The test is considered positive if the patient reports posterior pain. A negative test is indicated if the knee falls to the couch or aligns parallel with the opposite leg (9, 12).
• Compression Test: The patient lies on their side while the examiner places both hands over the upper iliac crest and applies downward pressure toward the floor. This force translates into anterior pressure on the sacrum. A positive result is indicated by pain in the SIJ, suggesting a possible lesion (9, 12).
• Thigh Thrust Test: With the patient in a supine position, the examiner stands on the opposite side and passively flexes the hip on the test side to 90 degrees. While palpating the SIJ with one hand, the examiner applies an axial thrust through the knee and hip. Reproduction of pain in the SIJ region indicates a positive test (12).
• Distraction Test: The patient lies supine, and the examiner stands facing them, applying a cross-handed outward and downward pressure on both ASISs. The test is positive if the patient reports unilateral gluteal or posterior leg pain (12).
• Gaenslen’s Test: The patient lies supine at the edge of the examination table with the test leg extended off the edge at the hip, while holding the opposite knee to the chest. The examiner applies downward pressure on the lower thigh of the extended leg and overpressure on the flexed knee. The test is considered positive if the patient experiences pain in the extended (test) leg (12).
2.4. Statistical Analysis
The collected data were summarized using descriptive statistics, including frequency, percentage, mean, and standard deviation. The Chi-square test or likelihood ratio test was applied to examine associations between the prevalence of dysfunction and variables such as age group, gender, level of proficiency, years of experience, and clinical test results. A p-value of less than 0.05 was considered statistically significant. All analyses were conducted using SPSS software (version 29.0.10; SPSS Inc., Chicago, IL).
3. Results
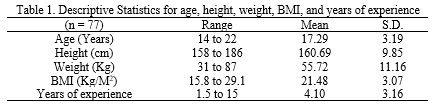
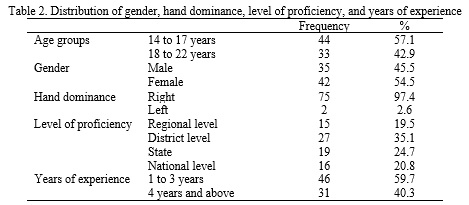
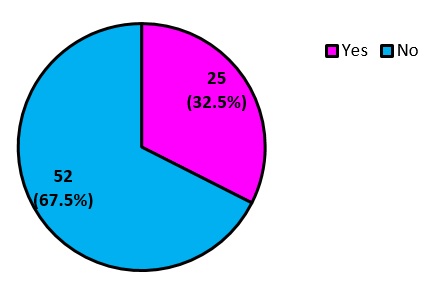
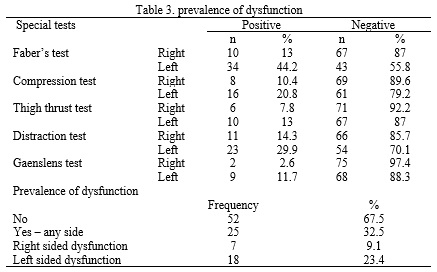
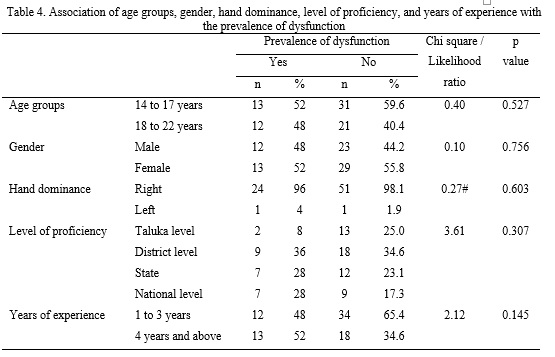
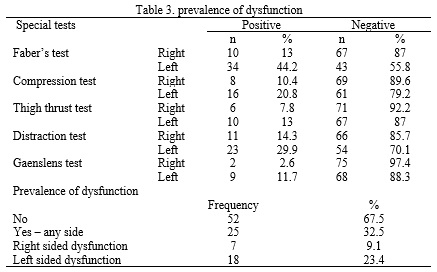
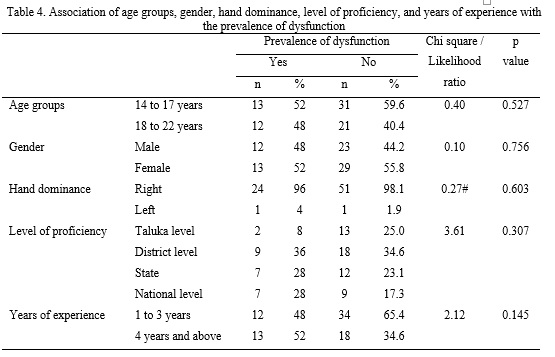
Tables 1 and 2 present the descriptive statistics and distribution of age, height, weight, BMI, years of experience, gender, hand dominance, and level of proficiency. In this study, the overall prevalence of sacroiliac joint (SIJ) dysfunction was found to be 32.5%, with 23.4% of the cases showing dysfunction on the left side and 9.1% on the right side (Fig. 1). Regarding individual clinical tests, the FABER test was positive in 44.2% of the left-sided cases and 13% of the right-sided cases. The compression test showed positive results in 20.8% on the left and 10.4% on the right. The thigh thrust test was positive in 13% on the left side and 7.8% on the right. For the distraction test, 29.9% of left-sided cases and 14.3% of right-sided cases reported pain. The Gaenslen’s test showed positive findings in 11.7% on the left side and 2.6% on the right. Based on the sample size, the 95% confidence interval for the overall prevalence was calculated to be between 22.3% and 44.1%, reflecting the likely range of true population prevalence within this group (Table 3). The Chi-square test or likelihood ratio test was used to assess the association between SIJ dysfunction and age group, gender, hand dominance, level of proficiency, and years of experience. No statistically significant associations were found between these variables and the prevalence of dysfunction, as all p-values were greater than 0.05 (Table 4).
Badminton is one of the most popular sports globally, with nearly 200 million individuals playing at various proficiency levels (1, 2). Known as the "fastest racket sport" due to its high tempo (2), badminton places unique demands on athletes. The game's rapid pace requires players to anticipate and react within fractions of a second, creating a dynamic and exhilarating environment (2, 3). As a physically demanding sport, badminton involves a wide range of movements that require speed, strength, agility, and explosive action. Players perform complex footwork patterns including lunging, pivoting, leaping, overhead smashes, sudden directional changes, and rapid acceleration and deceleration. These movements demand quick postural adjustments to maintain balance and prepare for subsequent shots (3). Such requirements impose substantial strain on the musculoskeletal system, particularly the trunk, lower extremities, and core muscles, which are constantly engaged during both offensive and defensive play (4). These biomechanical demands increase the risk of musculoskeletal injuries, especially among younger athletes (2).
Previous studies have reported that badminton players face an injury rate of approximately 0.85 injuries per year, 1.6–2.9 injuries per 1,000 hours of play, 2–5 injuries per 1,000 players, and account for 1%–5% of all sports-related injuries (5, 6). Of these, 58%–76% involve the lower limbs, 11%–16% the upper limbs, and 11%–16% the back (3, 7). The prevalence of low back pain (LBP) among badminton players has been estimated at 12.9% (4). Bhagat et al. (2022) (2) identified a significant prevalence of lower back and lower extremity injuries among badminton players in Vadodara, often linked to overuse, poor biomechanics, and inadequate fitness—factors also associated with sacroiliac joint dysfunction (SIJD). Similarly, Ejaz et al. (2023) (4) reported frequent musculoskeletal complaints, particularly in the lumbar spine, shoulders, and lower limbs, among players in Pakistan’s twin cities. These findings highlight the vulnerability of the lower back and pelvic regions in badminton athletes and suggest a potential underlying role of SIJ dysfunction. Despite these findings, research specifically addressing SIJD in badminton remains limited. In their comprehensive review of badminton-related injuries, Phomsoupha et al. (2020) (3) noted that although LBP is commonly reported, the SIJ is rarely identified as the specific source of pain. The SIJ is often overlooked in clinical evaluations due to diagnostic challenges and the overlap of symptoms with hip and lumbar spine disorders. However, considering badminton’s unique biomechanical demands—such as abrupt lunges, trunk rotations, and asymmetrical loading during rallies—the SIJ is likely subjected to significant mechanical stress (8, 9).
The importance of SIJD in the athletic context is further supported by Abdollahi et al. (2023) (9), who reported a strong correlation between SIJD and previous lower limb sports injuries. Their findings suggest that altered gait and loading patterns may increase SIJ stress (9, 10). This supports the concept of kinetic chain dysfunction and underscores the importance of evaluating SIJ integrity in athletes with recurrent leg, pelvic, or low back pain—particularly in young badminton players, who may adopt compensatory movement patterns due to ongoing musculoskeletal development. Sacroiliac joint dysfunction can significantly affect lower limb biomechanics, leading to pelvic asymmetry, restricted hip and knee mobility, and abnormal gait patterns, thereby increasing long-term injury risk (11). Early detection and intervention are crucial to preventing chronic pain and functional decline. The high-intensity demands of badminton can place substantial stress on the SIJ, making players more susceptible to dysfunction. Despite the joint's vital role in pelvic stability and load transmission, limited data exist regarding SIJD prevalence in badminton players (9).
This study aims to fill that gap. Determining the prevalence of SIJD among young badminton players can help identify sport-specific injury patterns. With such insights, targeted preventive strategies can be developed. Furthermore, early diagnosis of SIJD—given its impact on discomfort, mobility, and stability—can help optimize player performance. Ultimately, raising awareness among athletes, coaches, and healthcare professionals promotes a proactive approach to injury management and enriches the broader field of sports medicine.
2. Methods
2.1. Subjects
A cross-sectional study was carried out among badminton players in Belagavi city from November 2024 to May 2025, resulting in a final sample size of 77 participants. The required sample size was calculated using the standard formula:
n = [2(Zₐ + Zᵦ)² × p × q] / d²,
where n represents the sample size, Zₐ is the standard normal deviate corresponding to the desired confidence level (1.96 for 5%), Zᵦ denotes the standard normal deviate associated with the desired power (0.84 for 80%), p is the estimated prevalence (45%), q is 1 minus p (i.e., 55%), and d is the clinically meaningful effect size, set at 22.5%. By substituting these values into the formula, the calculated sample size was 77.
The estimated prevalence of 45% was selected based on previous literature addressing musculoskeletal dysfunctions such as low back pain and sacroiliac joint dysfunction (SIJD) in adolescent athletes. Although specific prevalence data for SIJD among badminton players is limited, studies involving similar athletic populations—such as runners, football players, and adolescent athletes in general—report prevalence rates ranging from 30% to 50%. Therefore, a midpoint estimate of 45% was deemed both conservative and realistic. The effect size of 22.5% was chosen based on two key considerations: first, the exploratory nature of this study as one of the earliest investigations into SIJD prevalence in adolescent badminton players, justifying a broader margin of error; and second, feasibility constraints, since detecting smaller effect sizes (e.g., 10–15%) would have required a substantially larger sample size, which was not practical due to the limited number of registered players in the region. Although 22.5% slightly exceeds the typical range of 10–20%, it was considered acceptable for an initial prevalence study with moderate statistical power.
Eligible participants were male and female badminton players aged between 14 and 22 years, each with at least 1.5 to 2 years of playing experience and a minimum of three training sessions per week on synthetic surfaces. Players with a body mass index (BMI) greater than 15 kg/m² were included, and only those who provided signed informed consent (or assent in the case of minors) were enrolled in the study. Exclusion criteria included active low back or buttock pain (e.g., due to prolapsed intervertebral disc or sciatica), recent fractures, lower limb injuries or surgeries within the past six months, and any diagnosed neurological or cardiovascular conditions.
2.2. Procedure
Prior to the commencement of the study, ethical clearance was obtained from the Institutional Ethics Review Committee. The study was also registered with the Clinical Trials Registry – India (CTRI), under the registration number CTRI/2024/12/077547. The study began by identifying the total number of badminton academies in Belagavi, from which two academies were selected randomly. Participants were screened based on the inclusion and exclusion criteria, and simple random sampling was used to select individuals from the list of registered players at each academy. The purpose of the study was clearly explained to each selected participant, and informed consent or assent was obtained prior to participation.
2.3. Outcome Measures
SIJD was evaluated using five standardized special tests administered in random order. A diagnosis of dysfunction was considered positive if three or more tests yielded positive results. Previous studies have shown that having three or more positive maneuvers provides a sensitivity of 94% and a specificity of 78% for diagnosing SIJ dysfunction. The tests used were Patrick’s FABER test, compression test, thigh thrust test, distraction test, and Gaenslen’s test (9, 10, 12). A test was deemed positive if it reproduced the subject’s familiar pain or discomfort in the SIJ region during the maneuver.
Descriptions of the SIJ Clinical Tests:
• Patrick’s FABER Test: The patient lies in a supine position while the examiner stands beside them. The examiner brings the ipsilateral hip into flexion, abduction, and external rotation, with the knee flexed so the heel rests on the contralateral knee. The examiner stabilizes the contralateral anterior superior iliac spine (ASIS) and applies posteriorly directed pressure to the flexed knee. The test is considered positive if the patient reports posterior pain. A negative test is indicated if the knee falls to the couch or aligns parallel with the opposite leg (9, 12).
• Compression Test: The patient lies on their side while the examiner places both hands over the upper iliac crest and applies downward pressure toward the floor. This force translates into anterior pressure on the sacrum. A positive result is indicated by pain in the SIJ, suggesting a possible lesion (9, 12).
• Thigh Thrust Test: With the patient in a supine position, the examiner stands on the opposite side and passively flexes the hip on the test side to 90 degrees. While palpating the SIJ with one hand, the examiner applies an axial thrust through the knee and hip. Reproduction of pain in the SIJ region indicates a positive test (12).
• Distraction Test: The patient lies supine, and the examiner stands facing them, applying a cross-handed outward and downward pressure on both ASISs. The test is positive if the patient reports unilateral gluteal or posterior leg pain (12).
• Gaenslen’s Test: The patient lies supine at the edge of the examination table with the test leg extended off the edge at the hip, while holding the opposite knee to the chest. The examiner applies downward pressure on the lower thigh of the extended leg and overpressure on the flexed knee. The test is considered positive if the patient experiences pain in the extended (test) leg (12).
2.4. Statistical Analysis
The collected data were summarized using descriptive statistics, including frequency, percentage, mean, and standard deviation. The Chi-square test or likelihood ratio test was applied to examine associations between the prevalence of dysfunction and variables such as age group, gender, level of proficiency, years of experience, and clinical test results. A p-value of less than 0.05 was considered statistically significant. All analyses were conducted using SPSS software (version 29.0.10; SPSS Inc., Chicago, IL).
3. Results
Tables 1 and 2 present the descriptive statistics and distribution of age, height, weight, BMI, years of experience, gender, hand dominance, and level of proficiency. In this study, the overall prevalence of sacroiliac joint (SIJ) dysfunction was found to be 32.5%, with 23.4% of the cases showing dysfunction on the left side and 9.1% on the right side (Fig. 1). Regarding individual clinical tests, the FABER test was positive in 44.2% of the left-sided cases and 13% of the right-sided cases. The compression test showed positive results in 20.8% on the left and 10.4% on the right. The thigh thrust test was positive in 13% on the left side and 7.8% on the right. For the distraction test, 29.9% of left-sided cases and 14.3% of right-sided cases reported pain. The Gaenslen’s test showed positive findings in 11.7% on the left side and 2.6% on the right. Based on the sample size, the 95% confidence interval for the overall prevalence was calculated to be between 22.3% and 44.1%, reflecting the likely range of true population prevalence within this group (Table 3). The Chi-square test or likelihood ratio test was used to assess the association between SIJ dysfunction and age group, gender, hand dominance, level of proficiency, and years of experience. No statistically significant associations were found between these variables and the prevalence of dysfunction, as all p-values were greater than 0.05 (Table 4).
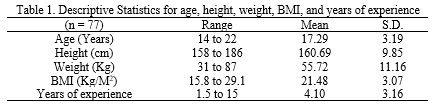
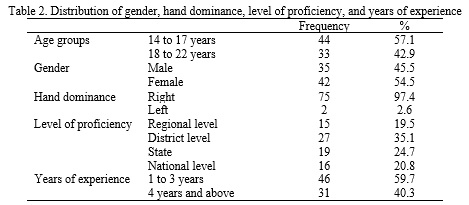
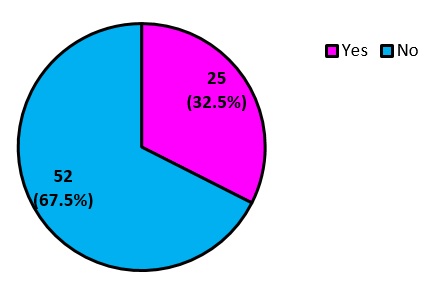
Fig.1. Prevalence of SIJ dysfunction
4. Discussion
According to the findings of this study, 32.5% of young badminton players had sacroiliac joint dysfunction (SIJD), with the majority of cases affecting the left side. In badminton, frequent lunges, trunk rotations, and unilateral weight-bearing actions expose the SIJ to cyclical shear and compression forces. These stresses are intensified by the sport’s fast-paced nature, where players repeatedly perform abrupt, asymmetrical movements.
Although the FABER test was positive in 34 participants on the left side (44.2%), the overall confirmed prevalence of SIJD on the left was 23.4% (n = 18). This discrepancy is explained by the diagnostic criterion requiring three or more positive special tests to confirm SIJD. A single positive FABER test alone is insufficient for diagnosis, as it may detect other sources of pain, such as hip joint or soft tissue pathology. Therefore, while the FABER test demonstrated high sensitivity, it lacked adequate specificity when used in isolation (9). The high prevalence of left-sided SIJD (23.4%) corresponds with the typical movement patterns of right-handed athletes, who predominantly generate force through their dominant side, leading to repeated torsional loading of the contralateral (left) SIJ during deceleration and pivoting movements. Since 97.4% of participants in this study were right-handed, this asymmetrical loading explains the left-sided dominance of SIJD (3, 10, 13).
SIJD is rarely an isolated issue; rather, it is often the result of broader kinetic chain disturbances (11, 12). SIJ dysfunction can cause pelvic misalignment, leading to compensatory overactivation or inhibition of surrounding muscles such as the gluteus maximus, hamstrings, and hip rotators. As biomechanical efficiency declines, players may unconsciously adjust foot placement, trunk posture, and knee alignment to compensate, increasing the risk of overuse injuries in the lumbar spine, knees, and ankles.
Adolescent athletes with poor core and pelvic neuromuscular control are more susceptible to SIJD. SIJ stability depends on a complex interaction between form closure (bony congruence) and force closure (muscle and ligament tension). During badminton play, imbalances in local stabilizers—such as the transverse abdominis, pelvic floor, and multifidus—can compromise force closure, especially under multidirectional loading. Repetitive micro-instabilities may strain the joint capsules and ligaments, contributing to persistent SIJ dysfunction (1, 9, 13).
Ejaz et al. (4) reported a high incidence of musculoskeletal discomfort among badminton players, particularly in the lower back, shoulders, and lower limbs, which supports the findings of this study. These regions are functionally interconnected, and dysfunction in one area often reflects or contributes to issues in another. The frequent unilateral and rotational movements in badminton likely lead to asymmetric loading of the SIJ. Ejaz et al.’s integrative rehabilitation approach highlights the interconnectedness of the musculoskeletal system and reinforces the critical role of the SIJ in load transmission and postural alignment during sports performance (13). Older epidemiological studies, such as those by Hoy et al. (1994) and Fahlström et al. (1998), found that up to 16% of badminton-related injuries involved the lower back. However, they did not specifically identify SIJD as a distinct diagnosis. The present findings contribute to this knowledge by identifying SIJD more precisely, suggesting that a substantial proportion of previously reported low back injuries may have involved the sacroiliac joint. Greater diagnostic precision can lead to more targeted treatment and rehabilitation strategies (5, 7).
Both the current study and a previous study by Naserpour et al. (14) on ankle injuries in karate athletes emphasize the importance of sport-specific biomechanics in joint health. High-intensity actions such as lunging, trunk rotation, and pivoting result in recurrent loading and mechanical stress on both the sacroiliac and ankle joints. These studies highlight the role of kinetic chain disruption, where dysfunction in one joint affects other joints. While Naserpour et al. associated ankle injuries with proximal instability, this study shows that pelvic dysfunction alters lower limb mechanics, thus increasing injury risk. These insights emphasize the importance of comprehensive biomechanical assessment and preventive strategies that account for inter-joint coordination in high-demand sports (14).
The implications for performance and injury prevention are significant. SIJD can alter pelvic alignment, leading to compensatory movement patterns that impair hip and knee function and contribute to overuse injuries elsewhere in the body. Early detection and management of SIJD can help prevent chronic pain and functional impairment (15). The findings of this study are consistent with those of Fatahi et al. (2022), who conducted a systematic review of badminton-related injuries. Their analysis showed that both acute and overuse injuries primarily affect the lower back, knees, and ankles, especially in amateur and adolescent athletes. These are the same anatomical regions often impacted by SIJD, supporting the notion that the mechanical demands of badminton place disproportionate stress on the lumbopelvic region (16). This supports the recommendation for structured preventive interventions that include core stability training, movement retraining, and surface adaptation. Integrating such evidence from larger-scale studies ensures that future injury prevention protocols are evidence-based, sport-specific, and comprehensive in addressing the multifactorial nature of SIJD in badminton players. Although core strength was not assessed in the present study, its role in SIJD remains an important area of inquiry. It is hypothesized that poor core stability may impair force closure, especially during high-intensity movements. Future studies should directly evaluate this relationship.
This study has several limitations that affect the depth and generalizability of its findings. Its cross-sectional design prevents conclusions about causality, and the absence of longitudinal follow-up limits understanding of the progression of sacroiliac joint dysfunction (SIJD). The diagnosis relied solely on clinical tests without imaging confirmation or biomechanical analysis, which may have resulted in underdiagnosis or failure to identify contributing factors. Important variables such as training intensity, history of previous injuries, and specific movement patterns were not controlled. Additionally, the study did not assess pain severity or the functional impact of SIJD. The use of convenience sampling from only two academies also limits the generalizability of the results. Finally, the lack of intervention or management recommendations further restricts the clinical applicability of the findings.
5. Conclusion
This study highlights a significant prevalence (32.5%) of sacroiliac joint dysfunction (SIJD) among young badminton players, with a higher occurrence on the left side. The findings emphasize the impact of the sport’s dynamic and asymmetrical movements on pelvic stability. Although no significant associations were found with demographic or training-related variables, the results underscore the importance of early screening and intervention. Recognizing and managing SIJD is essential to prevent chronic dysfunction, optimize performance, and reduce injury risk in adolescent athletes participating in high-intensity sports like badminton. Future studies should adopt longitudinal designs incorporating biomechanical analysis and imaging to enhance diagnostic accuracy and monitor the progression of SIJD. Including additional variables such as training intensity, core stability, and injury history may help identify risk factors more precisely. Research should also focus on the development of preventive and rehabilitative strategies and include larger, more diverse samples to improve generalizability. The use of standardized outcome measures like the Oswestry Disability Index (ODI) or the Roland-Morris Questionnaire is also recommended for future investigations.
Acknowledgments
I would like to thank KLE University's Institute of Physiotherapy, Belagavi, for allowing me to conduct this study.
Ethical Considerations
Compliance with ethical guidelines
Ethical clearance was obtained from the Institutional Ethics Review Committee. Informed consent/assent was obtained from the participants.
Funding
This research did not receive any grants from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Rochelle F Diniz: Concept and study design, data collection, drafting of the manuscript.
Dhaval Chivate: Concept and study design, data analysis and interpretation, critical revision for important intellectual content.
Basavaraj Motimath: Concept and study design, data analysis and interpretation, critical revision for important intellectual content.
All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Conflicts of interest
The authors declare no conflict of interest.
According to the findings of this study, 32.5% of young badminton players had sacroiliac joint dysfunction (SIJD), with the majority of cases affecting the left side. In badminton, frequent lunges, trunk rotations, and unilateral weight-bearing actions expose the SIJ to cyclical shear and compression forces. These stresses are intensified by the sport’s fast-paced nature, where players repeatedly perform abrupt, asymmetrical movements.
Although the FABER test was positive in 34 participants on the left side (44.2%), the overall confirmed prevalence of SIJD on the left was 23.4% (n = 18). This discrepancy is explained by the diagnostic criterion requiring three or more positive special tests to confirm SIJD. A single positive FABER test alone is insufficient for diagnosis, as it may detect other sources of pain, such as hip joint or soft tissue pathology. Therefore, while the FABER test demonstrated high sensitivity, it lacked adequate specificity when used in isolation (9). The high prevalence of left-sided SIJD (23.4%) corresponds with the typical movement patterns of right-handed athletes, who predominantly generate force through their dominant side, leading to repeated torsional loading of the contralateral (left) SIJ during deceleration and pivoting movements. Since 97.4% of participants in this study were right-handed, this asymmetrical loading explains the left-sided dominance of SIJD (3, 10, 13).
SIJD is rarely an isolated issue; rather, it is often the result of broader kinetic chain disturbances (11, 12). SIJ dysfunction can cause pelvic misalignment, leading to compensatory overactivation or inhibition of surrounding muscles such as the gluteus maximus, hamstrings, and hip rotators. As biomechanical efficiency declines, players may unconsciously adjust foot placement, trunk posture, and knee alignment to compensate, increasing the risk of overuse injuries in the lumbar spine, knees, and ankles.
Adolescent athletes with poor core and pelvic neuromuscular control are more susceptible to SIJD. SIJ stability depends on a complex interaction between form closure (bony congruence) and force closure (muscle and ligament tension). During badminton play, imbalances in local stabilizers—such as the transverse abdominis, pelvic floor, and multifidus—can compromise force closure, especially under multidirectional loading. Repetitive micro-instabilities may strain the joint capsules and ligaments, contributing to persistent SIJ dysfunction (1, 9, 13).
Ejaz et al. (4) reported a high incidence of musculoskeletal discomfort among badminton players, particularly in the lower back, shoulders, and lower limbs, which supports the findings of this study. These regions are functionally interconnected, and dysfunction in one area often reflects or contributes to issues in another. The frequent unilateral and rotational movements in badminton likely lead to asymmetric loading of the SIJ. Ejaz et al.’s integrative rehabilitation approach highlights the interconnectedness of the musculoskeletal system and reinforces the critical role of the SIJ in load transmission and postural alignment during sports performance (13). Older epidemiological studies, such as those by Hoy et al. (1994) and Fahlström et al. (1998), found that up to 16% of badminton-related injuries involved the lower back. However, they did not specifically identify SIJD as a distinct diagnosis. The present findings contribute to this knowledge by identifying SIJD more precisely, suggesting that a substantial proportion of previously reported low back injuries may have involved the sacroiliac joint. Greater diagnostic precision can lead to more targeted treatment and rehabilitation strategies (5, 7).
Both the current study and a previous study by Naserpour et al. (14) on ankle injuries in karate athletes emphasize the importance of sport-specific biomechanics in joint health. High-intensity actions such as lunging, trunk rotation, and pivoting result in recurrent loading and mechanical stress on both the sacroiliac and ankle joints. These studies highlight the role of kinetic chain disruption, where dysfunction in one joint affects other joints. While Naserpour et al. associated ankle injuries with proximal instability, this study shows that pelvic dysfunction alters lower limb mechanics, thus increasing injury risk. These insights emphasize the importance of comprehensive biomechanical assessment and preventive strategies that account for inter-joint coordination in high-demand sports (14).
The implications for performance and injury prevention are significant. SIJD can alter pelvic alignment, leading to compensatory movement patterns that impair hip and knee function and contribute to overuse injuries elsewhere in the body. Early detection and management of SIJD can help prevent chronic pain and functional impairment (15). The findings of this study are consistent with those of Fatahi et al. (2022), who conducted a systematic review of badminton-related injuries. Their analysis showed that both acute and overuse injuries primarily affect the lower back, knees, and ankles, especially in amateur and adolescent athletes. These are the same anatomical regions often impacted by SIJD, supporting the notion that the mechanical demands of badminton place disproportionate stress on the lumbopelvic region (16). This supports the recommendation for structured preventive interventions that include core stability training, movement retraining, and surface adaptation. Integrating such evidence from larger-scale studies ensures that future injury prevention protocols are evidence-based, sport-specific, and comprehensive in addressing the multifactorial nature of SIJD in badminton players. Although core strength was not assessed in the present study, its role in SIJD remains an important area of inquiry. It is hypothesized that poor core stability may impair force closure, especially during high-intensity movements. Future studies should directly evaluate this relationship.
This study has several limitations that affect the depth and generalizability of its findings. Its cross-sectional design prevents conclusions about causality, and the absence of longitudinal follow-up limits understanding of the progression of sacroiliac joint dysfunction (SIJD). The diagnosis relied solely on clinical tests without imaging confirmation or biomechanical analysis, which may have resulted in underdiagnosis or failure to identify contributing factors. Important variables such as training intensity, history of previous injuries, and specific movement patterns were not controlled. Additionally, the study did not assess pain severity or the functional impact of SIJD. The use of convenience sampling from only two academies also limits the generalizability of the results. Finally, the lack of intervention or management recommendations further restricts the clinical applicability of the findings.
5. Conclusion
This study highlights a significant prevalence (32.5%) of sacroiliac joint dysfunction (SIJD) among young badminton players, with a higher occurrence on the left side. The findings emphasize the impact of the sport’s dynamic and asymmetrical movements on pelvic stability. Although no significant associations were found with demographic or training-related variables, the results underscore the importance of early screening and intervention. Recognizing and managing SIJD is essential to prevent chronic dysfunction, optimize performance, and reduce injury risk in adolescent athletes participating in high-intensity sports like badminton. Future studies should adopt longitudinal designs incorporating biomechanical analysis and imaging to enhance diagnostic accuracy and monitor the progression of SIJD. Including additional variables such as training intensity, core stability, and injury history may help identify risk factors more precisely. Research should also focus on the development of preventive and rehabilitative strategies and include larger, more diverse samples to improve generalizability. The use of standardized outcome measures like the Oswestry Disability Index (ODI) or the Roland-Morris Questionnaire is also recommended for future investigations.
Acknowledgments
I would like to thank KLE University's Institute of Physiotherapy, Belagavi, for allowing me to conduct this study.
Ethical Considerations
Compliance with ethical guidelines
Ethical clearance was obtained from the Institutional Ethics Review Committee. Informed consent/assent was obtained from the participants.
Funding
This research did not receive any grants from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Rochelle F Diniz: Concept and study design, data collection, drafting of the manuscript.
Dhaval Chivate: Concept and study design, data analysis and interpretation, critical revision for important intellectual content.
Basavaraj Motimath: Concept and study design, data analysis and interpretation, critical revision for important intellectual content.
All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Conflicts of interest
The authors declare no conflict of interest.
Type of Study: Research |
Subject:
General
Received: 2025/07/7 | Accepted: 2025/08/1 | Published: 2025/08/2
Received: 2025/07/7 | Accepted: 2025/08/1 | Published: 2025/08/2
References
1. Shedge SS, Ramteke SU, Samal S. Integrated Rehabilitation Approach Utilizing Swiss Ball Training, Mulligan Taping, and Mobilization with Movement for Simultaneous Management of Sacroiliac Joint Dysfunction and Lateral Ankle Sprain in a Badminton Athlete: A Case Study. Cureus. 2024;26;16(3):e56942. [DOI:10.7759/cureus.56942]
2. Bhagat C, Sarvanan M, Bhura P. Prevalence of musculoskeletal injuries among badminton players of Vadodara. International Journal of Physical Education, Sports and Health. 2022;9(5):161-163.
3. Phomsoupha M, Laffaye G. Injuries in badminton: A review. Science & Sports. 2020;35(4):189-99. [DOI:10.1016/j.scispo.2020.01.002]
4. Ejaz R, Farooq MN, Amjad F, Batool R, Khalil H, Tasnim A, et al. Prevalence of Musculo-Skeletal Pain among Badminton Players in Twin Cities of Pakistan: Prevalence of Musculo-Skeletal Pain. THE THERAPIST (Journal of Therapies & Rehabilitation Sciences). 2023;4(4):14-8. [DOI:10.54393/tt.v4i04.176]
5. Høy K, Lindblad BE, Terkelsen CJ, Helleland HE. Badminton injuries--a prospective epidemiological and socioeconomic study. British Journal of Sports Medicine. 1994;28(4):276-9. [DOI:10.1136/bjsm.28.4.276] [PMID]
6. Boesen AP, Boesen MI, Koenig MJ, Bliddal H, Torp-Pedersen S, Langberg H. Evidence of accumulated stress in Achilles and anterior knee tendons in elite badminton players. Knee Surgery, Sports Traumatology, Arthroscopy. 2011;19(1):30-7. [DOI:10.1007/s00167-010-1208-z] [PMID]
7. Fahlström M, Björnstig U, Lorentzon R. Acut badminton injuries. Scandinavian journal of medicine & science in sports. 1998;8(3):145-8. [DOI:10.1111/j.1600-0838.1998.tb00184.x]
8. García-Peñalver UJ, Palop-Montoro MV, Manzano-Sánchez D. Effectiveness of the muscle energy technique versus osteopathic manipulation in the treatment of sacroiliac joint dysfunction in athletes. International Journal of Environmental Research and Public Health. 2020;17(12):4490. [DOI:10.3390/ijerph17124490] [PMID]
9. Abdollahi S, Sheikhhoseini R, Rahimi M, Huddleston WE. The sacroiliac dysfunction and pain is associated with history of lower extremity sport related injuries. BMC sports science, medicine and rehabilitation. 2023;15(1):36. [DOI:10.1186/s13102-023-00648-w] [PMID]
10. Yavuz F, Kelle B, Balaban B. The interventional pain management of sacroiliac joint pain: A brief review. Journal of Advanced Neuroscience Research. 2015;2:25-9. [DOI:10.15379/2409-3564.2015.02.02.5]
11. Feeney DF, Capobianco RA, Montgomery JR, Morreale J, Grabowski AM, Enoka RM. Individuals with sacroiliac joint dysfunction display asymmetrical gait and a depressed synergy between muscles providing sacroiliac joint force closure when walking. Journal of Electromyography and Kinesiology. 2018;43:95-103. [DOI:10.1016/j.jelekin.2018.09.009] [PMID]
12. Manske RC, Magee DJ. Orthopedic physical assessment. 7th ed. St. Louis: Elsevier Health Sciences; 2020.
13. Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. Journal of anatomy. 2012;221(6):537-67. [DOI:10.1111/j.1469-7580.2012.01564.x] [PMID]
14. Naserpour H, Mirjani M. An investigation of ankle injury prevalence and its mechanism among Iranian Professional Karateka. Journal of Sport Biomechanics. 2019;4(4):2-15. [DOI:10.32598/biomechanics.4.4.2]
15. Hu H, Meijer OG, Van Dieen JH, Hodges PW, Bruijn SM, Strijers RL, et al. Muscle activity during the active straight leg raise (ASLR), and the effects of a pelvic belt on the ASLR and on treadmill walking. Journal of biomechanics. 2010;43(3):532-9. [DOI:10.1016/j.jbiomech.2009.09.035] [PMID]
16. Fatahi A, Hamzeh L, Molaviaan R, Dehnavi M. Badminton Injuries: A Systematic Review. Journal of Sport Biomechanics. 2022;8(1):16-33. [DOI:10.52547/JSportBiomech.8.1.1]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |